Graduating in a Year Like No Other
From an unexpected hiatus to babysitting for healthcare workers, the past year has brought plenty of new experiences for medical students graduating this spring from the Temerty Faculty of Medicine.
But with these experiences came new skills and the discovery of a deep resiliency that the class of 2T1 will take into their medical careers.
As the cohort of 254 MD graduands prepares for what’s next — convocation celebrations, licensing exams and residency placements — class co-presidents Prem Nichani and Ward Al-far look back on a year unlike any other.
Stepping Up
In the spring of 2020, pandemic safety protocols put the class of 2T1 on temporary hiatus from clerkship rotation. During three months of unexpected downtime, the MD students stepped up to volunteer with initiatives to support health care systems and the community. Students organized PPE collection drives, worked crisis support telephone services, filled hospital screening and public health contact tracing roles, and pitched in to offer childcare and grocery delivery services to frontline healthcare workers.
A New Landscape
When clinical rotations resumed in July 2020, the MD students found themselves in a medical landscape transformed by new safety protocols, new routines for health care teams and a new relationship with patients for the physicians-in-training.
Al-far provided one-on-one medical care to patients, and found himself managing the social needs of patients who couldn’t have family members nearby due to safety protocols.
“You might find yourself supporting a scared breast cancer patient who can’t have her mother with her,” he said. “That adds a lot more emotional and social responsibility to caring for people, but the difference it makes for the patient is huge."
Al-far describes the experience as “intense” but says it solidified the communication and patient advocacy skills he will carry into his future practice.
As healthcare adapted to the changing demands of COVID-19, the new protocols also gave learners an atypical view of the specialities they might be considering.
“This is a formative period,” said Al-far of the truncated Clerkship placements that give MD students a chance to experience different medical disciplines before deciding on their speciality.
The circumstances also shifted how learners prepared for residency placements. Travel restrictions meant the 2T1 class had to find new ways to explore the cities and institutions where they hoped to land residency placements.
“This is where we will spend the next five years and maybe set up our practices and our lives,” said Nichani.
Despite the challenges, MD Program Foundations director Marcus Law says the past year gave this cohort a unique opportunity to put their pre-clerkship training into practice.
“They observed how physicians learn and manage uncertainties and ambiguities,” said Law. “They also deepened their understanding of how to adapt to the unknown with new knowledge and to how to apply a health equity lens to advocate for their patients with COVID.”
“This class has developed life skills that will help them manage the next crisis,” he continued. “They’ve risen to the challenge and will be ready to tackle what comes next.”
In it Together
Through it all, the class of 2T1 leaned on each other, met safely outdoors when in-person visits were permitted and moved online when they were not. There were virtual town halls with faculty to keep students informed of changes and online counseling sessions offered through the Office of Health Professions Student Affairs.
The co-presidents also helped the class safely mark milestones and make new memories together. They recently hosted the first-ever virtual match party to celebrate residency matches and are preparing for an online convocation to take place Tuesday, June 15.
Future Forward
With classes behind them, many in the 2T1 cohort are preparing for licensing exams and making relocation plans to begin their residency placements on July 1.
This period also typically offers opportunities for travel and rest, a break Nichani notes is especially needed after the intense pressures of the past year.
The co-presidents say their 2T1 classmates showed extraordinary determination and resiliency over the past year which will stand them in good stead in the future.
“Making it through these four years is a challenge itself, but with the pandemic, it’s a quite an accomplishment,” said Al-far, who will start residency in anesthesiology at McMaster University in July.
Nichani, who will remain in Toronto for his residency in ophthalmology, agrees. “Despite how hard this experience has been, it made our class stronger together and as individuals,” he said. “We’ve been through a heck of a lot.”
Vice Dean, Medical Education Patricia Houston lauded the class for their accomplishments and contributions.
“In addition to offering my congratulations the class of 2T1 on the successful completion of the MD Program, I also want to thank our newest graduates,” said Houston.
“Over the last year in particular, the class of 2T1 has stepped up to help in the clinical environment, assisted in caring safely for COVID patients and were a help to students in the other years of the program. It’s been a privilege to work with each of these students and I wish them the best as they embark upon the next chapter in their life long education journey.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

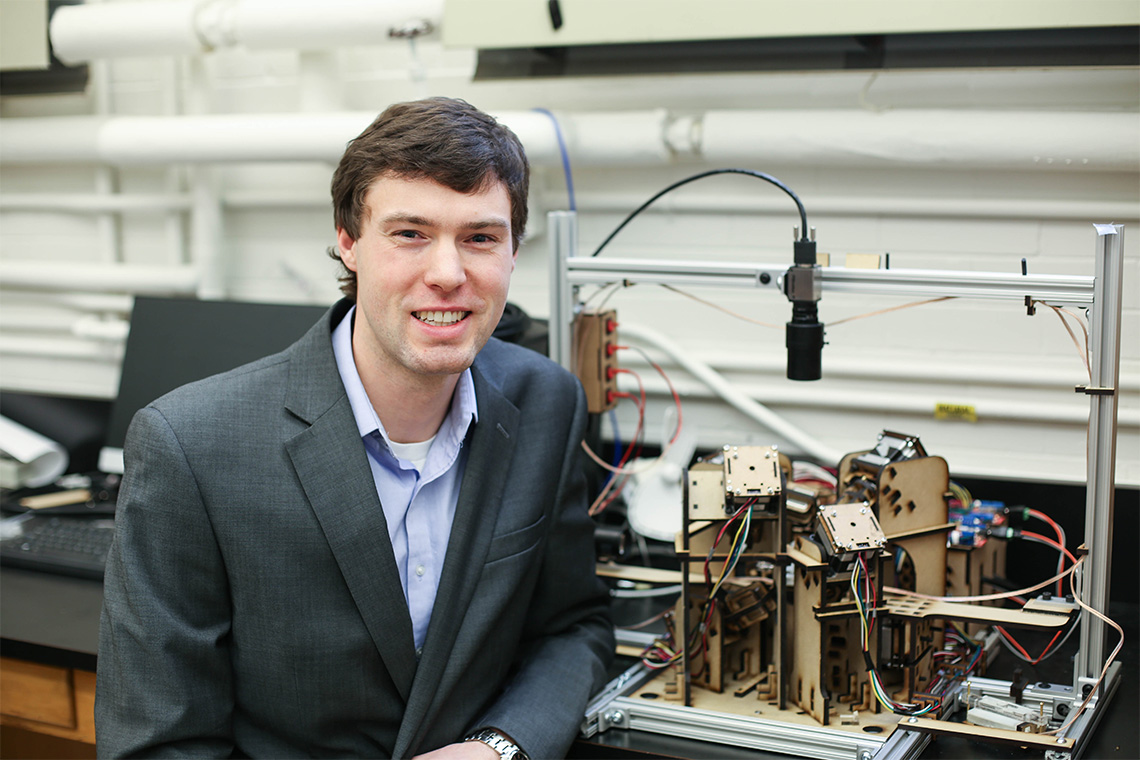
U of T Researchers Develop Microrobots to Conduct Minimally Invasive Brain Surgery
Researchers at the University of Toronto are developing microrobots, precisely controlled by magnetic fields, that could one day be used to perform minimally invasive brain surgery on children.
The research team – co-led by Eric Diller, an associate professor of mechanical engineering in the Faculty of Applied Science & Engineering, and James Drake, a professor in the department of surgery in the Temerty Faculty of Medicine and a pediatric neurosurgeon at the Hospital for Sick Children (SickKids) – says the technology represents a departure from the rigid, wired designs of most micro-surgical tools.
“Advancing surgery through an endoscope in the pediatric brain requires miniaturized versatile tools which can be precisely controlled,” says Drake. “This novel concept of using tiny, magnetized tools, controlled by robotic external magnets, shows great promise in addressing this need for both pediatric and adult patients.”
Each year 24,000 malignant brain tumours are detected in the United States. These tumours are the most common form of solid cancer in children, and surgery to remove the tumour is often the first recommended course of treatment. The surgeries can be highly invasive with a long recovery process. In some cases, when surgery via endoscope is possible, the tools may not be small or dexterous enough to perform the treatment.
Building on work by Drake and his team at the Wilfred and Joyce Posluns Centre for Image Guided Innovation and Therapeutic Intervention (PCIGITI), Diller and Drake brainstormed ideas for a research collaboration. Diller pitched the idea of magnetically driven neurosurgical tools. The project took off after funding was secured from the Canadian Institutes of Health Research (CIHR) and the Natural Sciences and Engineering Research Council of Canada (NSERC).
Diller and his team have been developing a prototype with tiny grippers mounted on the end of a flexible wire “wrist” and controlled by external magnetic fields. The tool features magnets on both the gripping forceps and the flexible wrist. As magnetic fields are applied, the tool will either open and close the grippers or move the wrist.
“For these surgical tools, we’re working at a very challenging scale of around one- to five-millimetre parts, with some materials that don’t work well with micro-machining processes,” says Cameron Forbrigger, a PhD candidate in the Faculty of Applied Science & Engineering. “As a result, we had to do a lot of the assembly of off-the-shelf magnets, plates and wires by hand with a laser welding system.
“If you’re not careful, the titanium wires could disintegrate under the laser beam.”
In tests performed on a rubber model of the brain with a simulated tumour, the gripper was able to successfully enter the ventricles of the brain and remove the tumour, controlled completely by external magnetic fields.
The researchers are now working on a second prototype of the gripping tool that features a simplified design to allow for more control over the forceps. The prototype magnetic tools are being developed to be about half the size of traditional surgical robot tools, which are about five millimetres across, while maintaining the same dexterity.
“Developing new technology for pediatric minimally invasive surgery – in this case neurosurgery – takes a collaborative team of engineers and surgeons. Our team from the department of mechanical and industrial engineering at U of T and PCIGITI at SickKids has been very successful in this regard,” says Drake.
There are still several steps to be taken before these microrobots are seen in the operating room. The team plans to create more tools, including micro scissors. They also need to determine the best way to generate magnetic fields in the operating room.
“Our next step will be to join our colleagues at SickKids for a simulation in vivo, which will provide the opportunity to see how these microrobots will function in the operating room, and to try different ways of setting up the magnetic coils,” Diller says.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
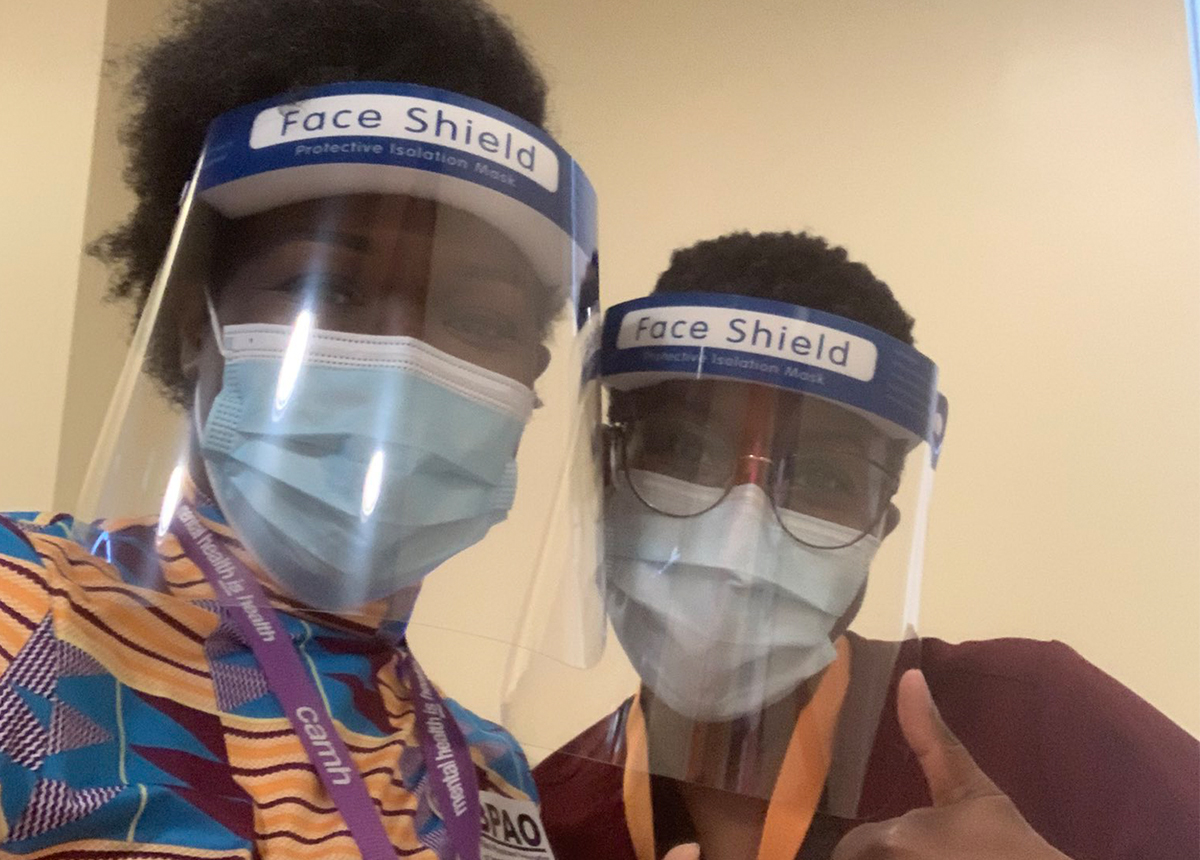
Family Doctors Help Lead Black Health Vaccine Initiative
The COVID-19 pandemic has had a disproportionate impact on racial and ethnic minority groups, with Black communities among those hit hardest.
To address this inequity, the Black Physicians’ Association of Ontario (BPAO) are leading the Black Health Vaccine Initiative, including family doctors from the Temerty Faculty of Medicine’s Department of Family and Community Medicine (DFCM).
The initiative aims to advocate, educate and vaccinate in Ontario’s Black communities.
“Black people are over-represented in front-line roles – in factories, as personal support workers and other essential services. Many don’t have the luxury of working from home, or the housing conditions to isolate when needed,” says Onye Nnorom, DFCM’s Equity, Diversity & Inclusion Lead and BPAO President.
In a position statement, the BPAO shared City of Toronto data from December 2020 showing COVID-19 rates and hospitalizations were three times higher for Black people who live in Toronto, compared with white people.
A Statistics Canada report from March 2021 indicates that 49 per cent of Canadians say they are not very likely to get a vaccine. For Black Canadians, this figure rises to 77 per cent.
Long-standing systemic health gaps and social inequities have put Black Canadians at higher risk of contracting COVID-19, says Nnorom, and underpin education, employment and income disparities.
A distrust of the COVID-19 vaccine, and public services in general, stems from centuries of anti-Black racism that has resulted in a systemic inequity of power, resources and opportunities that discriminates against people of African descent, she adds.
A key component of the Black Health Vaccine Initiative is the Network of Black Vaccinators (NBV) – Black and BIPOC physicians and working closely with community partners to build vaccine confidence and increase vaccine uptake in Black communities.
Duate Adegbite has been performing vaccinations at TAIBU Community Health Centre, as part of a clinic that officially launched in April with support from Scarborough Health Network and DFCM.
The clinic serves primarily Black, Indigenous and Francophone communities, as well as the local Malvern community.
“The clinic has been a culturally safe space for people to get vaccinated,” says Adegbite, a lecturer in DFCM and physician NBV lead at TAIBU.
“We’ve had many patients come in and say they’ve never seen so many Black doctors. This creates a level of comfort because people see themselves reflected in who’s providing their care – from administrative staff, to doctors and nurses,” says Adegbite, a family doctor at the Toronto Western Family Health Team.
Dominick Shelton, an assistant professor in DFCM and co-lead for the Black Vaccinators Network, says the response to vaccinations at TAIBU has been fantastic.
“Black and other racialized physicians are helping to overcome vaccine hesitancy in Black communities. We are having the important conversations with people and our mere presence as a vaccinator is sending a message of confidence in the COVID vaccine,” says Shelton, an emergency physician at Sunnybrook Health Sciences Centre.
The Black Health Vaccine Initiative is currently focused on pop-up clinics in hot-spot neighbourhoods.
The first of these pop-ups will be hosted with the Jamaican Canadian Association the weekend of May 8 and 9, in partnership with Black Creek Community Health Centre. Additional pop-ups will follow across the city, in Peel and beyond.
To reach and vaccinate those that are hardest hit, community partnerships are key, say faculty involved in the project.
“Community health centres already have established relationships and are trusted by the communities they serve,” says Adegbite, who has been a BPAO member since being in the U of T MD Program over 10 years ago.
“Getting information from someone who you trust helps to dispel vaccine hesitancy. Working at community centres, we have more time to sit and talk with people who have questions.”
David Esho, an assistant professor in DFCM, is leading the mobile and pop-up vaccine clinics in Toronto as part of the Black Health Vaccine Initiative.
“We are very aware of vaccine distrust and hesitancy in Black communities, so we’re working to recruit Black health professionals to act as vaccinators and educators,” says Esho, who is also a family physician with the Toronto Western Family Health Team.
“I am very proud of the work we are doing at BPAO. We have focused on the importance of relationship building in our vaccination efforts and utilized our links with community agencies, DFCM and our hospital partners to bring vaccines to members of our community who may not otherwise have been able to access them.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Exploring All Sides of the Coin
More than 100 physiotherapy learners at the University of Toronto have created teaching resources they hope will help make their profession and the world more equitable.
The learners developed 65 arts-based teaching materials such as drawings, blog posts and video games to explore systems of inequality including racism, ableism and ageism.
The assignment is part of a cross-curricular theme called social, political, ethical and cultural (SPEC) dimensions of health and healthcare in the Master of Science in Physical Therapy program.
The idea is to deepen each learner’s understanding of equity, diversity and inclusion (EDI) and anti-oppression in physiotherapy and healthcare, and lay groundwork to transform the field of physiotherapy.
“There’s a lot of privilege in this profession from the composition of the classrooms to who has access to physiotherapy. We want learners to learn, unlearn, speak up, stand up, and make space for those who live on the margins,” says Stephanie Lurch, equity, anti-racism and social accountability leader in in the department of physical therapy at the Temerty Faculty of Medicine.
Lurch co-developed the project with Martine Quesnel, a professor of physical therapy at Temerty Medicine.
The goal is to help learners reflect critically on their own privilege and how it relates to interlocking systems of inequality using the 'coin model'. Each ‘coin’ represents a system of inequality, such as racism or ableism. Based on one’s social location, people either receive unearned advantage (top of the coin) and disadvantage (bottom of the coin) — even if they’re unaware of these dynamics.
“Often, people focus equity, diversity and inclusion issues on learning about the ‘bottom of the coin’, while ignoring the systems that create the inequality in the first place or the complicity of people on the top of these same coins,” says Stephanie Nixon, a professor of physical therapy and director of the International Centre for Disability and Rehabilitation who helped co-create the project with Lurch and Quesnel.
“We wanted to awaken our learners to the forms of unearned advantage, or privilege, they receive and how they can work to interrupt those harmful systems,” Nixon says.
For learners Andrew Daly and Diane Kim, developing their materials was transformative. Through their project, Dieting, a Piece of Cake? No Weigh!, the pair explored the ways sizeism affects people with bigger bodies in the healthcare system.
Their cartoon features a patient and their physiotherapist, who presents weight loss as a pillar of managing osteoarthritis. As the physiotherapist shares information about macronutrients and moderate-to-vigorous activity levels, the patient appears to feel uncomfortable and overwhelmed.
Daly and Kim draw the reader’s attention to how clinicians need to be aware of how they may be reproducing fat stigma while educating patients about potential benefits of weight loss.
“As clinicians, it can be uncomfortable to examine and discuss our own blindspots in these systems of inequality, like sizeism. This discomfort can be a barrier to talking about these issues, which means they don’t get challenged,” says Kim. “Our profession has such potential to optimize people’s lives. To have good clinical outcomes, we need to make sure we’re not unwittingly contributing to inequity.”
Students presented their projects at a gallery walk event that featured six curated exhibition discussions led by faculty members and community ‘guest stars’ who shared their own reflections on the resources, which helped deepen the conversations and further the students’ learning.
The assignment and event are part of the renewed physical therapy curriculum.
“When we were designing the project, we considered important curricular pieces,” says Quesnel. “But importantly, we asked ourselves, what does it take to be an exceptional physiotherapist?” Quesnel says they kept coming back to the idea of meaningful care — taking the entire individual into account and being creative.
“And we wanted to include people from the community because that’s who receives care,” Quesnel says. “They teach us more than we teach them.”
Lurch says that traditional lectures enable a colonial approach; students swoop in, take what they want, and leave. “There’s no reciprocity,” she says. “This format invites learners to take a more active role in engaging with the material and ultimately, change the system.”
Highlights from the Gallery Walk can be seen here.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Breakthrough Paves Way for More Cancer Patients to Benefit from Immunotherapy
Adoptive cell therapy is a promising cancer treatment that uses our immune system to eliminate cancer cells. These treatments, however, are only effective for a small subset of individuals with specific types of cancer and specific inherited genes. A recent breakthrough by Naoto Hirano, a professor in the Department of Immunology, paves the way for novel immunotherapies to help more patients, regardless of their genetic ancestry, live longer and healthier lives.
In a study published in Nature Biotechnology, Hirano and his collaborators developed a new technology that rigorously and robustly identifies the immune cells that are capable of recognizing and eliminating cancer cells. This technology allows researchers to develop new immunotherapies for cancer patients that are not limited by the differences – or heterogeneity – of tumour cells, thus expanding the potential impact of immunotherapy for patients around the world.
Hirano’s technology applies to an immunotherapy approach called T cell receptor (TCR) gene therapy that is based on genetically-engineered immune cells (T cells) recognizing and binding to specific molecules, called peptide-loaded human leukocyte antigens (HLA), on the surface of cancer cells. Although there has been progress in TCR therapy, there are more than 28,000 different variations of HLA found in humans and current TCR therapies only work for a few of these variations.
“Historically, TCR treatments have been developed for those who had the most common and well-studied HLA alleles, which often meant that these immunotherapies only worked for people from Caucasian ancestry,” says Hirano, who is also a senior scientist at the Princess Margaret Cancer Centre and Ontario Institute for Cancer Research clinician scientist. “It was an important goal for us to develop a technology that could work for a broad range of HLA alleles. We’re proud of what we developed because it could help many more cancer patients in the future.”
The technology presented in this study involves a methodology that can – in a single step at a low expense – form a functional protein structure, called a dimer, that is comprised of any peptide and HLA molecule, regardless of type, and can bind to and identify a variety of T cells. The method improves the binding affinity between T cells and HLA molecules nearly 200-fold relative to prior methods, which could allow researchers to better identify and engineer the T cells for novel immunotherapies.
The technology has been licensed to TCRyption Inc. for further development, translation, and large-scale implementation. In the future, it may be applied to fields other than cancer research and care, including autoimmune diseases such as rheumatoid arthritis and type 1 diabetes.
“I’m grateful for the cancer research community’s support over the years, which has enabled me to focus on important and challenging issues,” says Hirano, who was named the University Health Network’s Inventor of the Year last year for developing these analysis techniques. “Only with the support for rigorous experimentation, deep expertise, and innovative thinking, were we able to make this breakthrough.”
Learn more about the work behind this publication, or read more about Hirano.
Note: N.H. has received research funding from Takara Bio and served as a consultant for Takara. The University Health Network has filed a patent application related to this study on which N.H. is named as a lead inventor. N.H. is cofounder and has equity in TCRyption to which the technologies used in this study have been licensed.
This article was originally published by the Ontario Institute for Cancer Research.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Honouring Impact: 2021 Dean's Alumni Awards
Temerty Medicine alumni from across the clinical, fundamental science and rehab sectors have always worked tirelessly to meet the needs of their communities. This year, we were proud to recognize six individuals whose achievements and contributions to the advancement of health and health care stand out as truly extraordinary at a virtual event in May.
Honourees include a world-renowned epidemiologist, an occupational therapy visionary, a neuro-oncologist with more than 30 global health missions, an innovative quality improvement (QI) education expert, as well as a clinician and a researcher who are shaping our understanding of diabetes and its treatments. While their work may be diverse, they share an important attribute: a commitment to making a difference.
“The large number and strength of the nominations we received this year are a testament to the significance of these awards,” says Dean Trevor Young. “The recipients of the 2021 Dean's Alumni Awards exemplify everything that makes our alumni community so strong, vital, and ready to rise to any challenge.”
This year, the Temerty Faculty of Medicine is honouring:

Lifetime Achievement – International/Global Impact Award
Dr. Sharon Straus (MD ’90, PGME ’96, MSc ’03)
Dr. Straus is one of Canada’s top clinician-scientists, and has earned an international reputation in the fields of geriatrics and epidemiology and a wide range of honours for her clinical work, research and professionalism. She is the first female Physician-in-Chief at St. Michael’s Hospital in Toronto, where she also serves as director of the Knowledge Translation (KT) Program, and holds a Tier 1 Canada Research Chair in Knowledge Translation and Quality of Care. Dr. Straus has authored more than 500 publications and three textbooks in evidence-based medicine, knowledge translation and mentorship, and created unique courses in practising KT that are delivered worldwide. She currently leads an international network to build KT capacity in low- and middle-income countries, funded by the Canadian Institutes of Health Research (CIHR), World Health Organization (WHO) and the United Nations, and leads the WHO’s technical support centre for guideline implementation.

Lifetime Achievement - National/Community Impact Award
Professor Emerita Judith Friedland (Dip. POT ’60, BA ’76, MA ’81, PhD ’89)
Professor Emerita Judith Friedland has been a visionary and inspirational force in the field of occupational therapy for more than 40 years. She assumed academic leadership of U of T’s Division of Occupational Therapy in 1991 and established it as a full department within the Faculty of Medicine (now the Temerty Faculty of Medicine) in 1993. Overseeing changes to the curriculum and program structure, she laid the groundwork for an entry-level MScOT program which was implemented in 2001. Her 2011 book, Restoring the Spirit: The Beginnings of Occupational Therapy in Canada, 1890-1930, garnered national and international attention and led to a variety of speaking engagements and other initiatives. She has used her leadership skills to chair Research Ethics Boards at U of T and Public Health Ontario. Her own research activity, primarily in mental health, and her mentorship of others continue to this day.
Humanitarian Award
Dr. Mark Bernstein (BSc ’72, MD '76, PGME ’83, MHSc ’03)
Dr. Bernstein’s career is rich in humanitarian deeds as a neurosurgeon, researcher, medical educator, bioethicist and palliative care provider. He is a neurosurgeon specializing in neuro-oncology at the Toronto Western Hospital, as well as a home-based palliative care physician with The Temmy Latner Center for Palliative Care at Mount Sinai Hospital. In 2011, Dr. Bernstein was appointed UHN's Greg Wilkins-Barrick Chair in International Surgery. In the last two decades he has led over 30 missions to low- and middle-income countries to help patients and build capacity in neurosurgery and, more recently, in palliative care. Through the Wilkins-Barrick Chair, he funds fellowships to train neurosurgeons from low- and middle-income countries and supports two awards — a Women in Neurosurgery Award and a Visiting International Surgeon Award.

Emerging Leader Award
Dr. Brian Wong (BSc ’99, MD ’03, PGME '06, PGME ‘07)
Dr. Wong is a general internist at Sunnybrook Health Sciences Centre and a nationally and internationally-recognized quality improvement (QI) education expert who is leading truly transformative changes in our healthcare system. His work centres on the intersection between patient safety, quality improvement and medical education. He played an instrumental role in revising the CanMEDS 2015 competency framework to integrate QI and patient safety as required elements of training for all physicians in Canada. As Director of the Centre for Quality Improvement and Patient Safety (CQuIPS) — a joint partnership between U of T’s Temerty Faculty of Medicine and three of its affiliated hospitals — Dr. Wong has co-led the creation of several innovative educational programs. Most recently, in response to the COVID-19 pandemic, Dr. Wong co-led the creation of a new clinical program called LTC+ that partners long-term care (LTC) homes in Toronto with acute care hospitals and community services to increase clinical support in LTC homes.

Insulin 100 Emerging Leader Award (co-winner)
Dr. Kim Connelly (PGME ’09)
As a clinician, teacher and researcher at the nexus of diabetes and cardiology, Dr. Connelly has demonstrated unique and exceptional leadership. He is the Director of the Krembil Stem Cell Facility at St. Michael’s Hospital, where he uses cell-based therapies to improve cardiac and renal dysfunction as a result of diabetes. He has led Diabetes Canada’s Guidelines Steering Committee on Cardiovascular Complications and the Treatment of Diabetes in People with Heart Failure, as well as being the Chair of the Guidelines Committee for the Canadian Cardiovascular Society. Dr. Connelly has received many prestigious awards, including Young Investigator of the Year from the Canadian Cardiovascular Society, Ontario’s Early Researcher Award and a Canadian Institutes of Health Research (CIHR) New Investigator Award. He has also been recognized internationally for his work in heart failure in diabetes, most recently as a speaker at the American Diabetes Association’s 2020 Heart failure symposium.

Insulin 100 Emerging Leader Award (co-winner)
Dr. John Sievenpiper (MSc '00, PhD '04, PGME '10, PGME '12)
Dr. Sievenpiper has had tremendous influence on national and international guidelines and policies in the field of diabetes and nutrition. He initiated and drove a modernization of the clinical practice guidelines for diabetes, cardiovascular disease and obesity in Canada and Europe, shifting the guidance to focus more on quality over quantity and dietary patterns over single nutrients. He is also an expert committee member with Diabetes Canada, the European Association for the Study of Diabetes (EASD), Canadian Cardiovascular Society (CCS), and Obesity Canada. Through his work with the Lawson Centre for Child Nutrition, he transformed programming within U of T’s MD Program and Department of Nutritional Sciences, expanding the Nutrition theme and developing and leading the MD Program’s Lifestyle Medicine Week. This is the first program of its kind to be offered by a Canadian medical school, and provides instruction and application of healthy lifestyle behaviours, including cooking, stress management, sleep and physical activity.
Due to the COVID-19 pandemic, 2020 and 2021 award recipients were formally honoured at an intimate virtual celebration in May 2021. View the event recording.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Towards a Cure: Insulin100 Scientific Conference Draws World’s Leading Diabetes Researchers
Patient stories. Innovative diabetes therapies. A peek inside the bedroom of one of the scientists who discovered insulin at the University of Toronto.
Those were just a few highlights of U of T’s recent Insulin100 Scientific Symposium, which drew more than 6,000 attendees from around the world.
The two-day scientific symposium commemorated the 100th anniversary of the discovery of insulin in a U of T laboratory – and was preceded by a public celebration one day earlier that featured stirring videos from diabetes patients across the globe who spoke about the role of insulin in their lives.
“I’m thankful for insulin because it allows me to keep playing tennis,” said one U.S. woman. “I am thankful for insulin because even though I’m diabetic, it still means I can eat great food,” said a man from the U.K. “I’m thankful for insulin because I can travel,” a woman from New Zealand said.
In 1921, Ontario surgeon Frederick Banting, then-U of T student Charles Best and U of T alumnus James Collip, working under the direction of U of T physiology professor J.J.R. Macleod, extracted the peptide hormone that revolutionized diabetes treatment, making the metabolic disease manageable through insulin.
Attendees at the public celebration also received an account – delivered by the curator of the Banting House in London, Ont. – of the moment Banting arrived at his world-changing idea in the middle of the night, complete with a photo of his wallpapered bedroom.
Yet, as Banting himself said during the lecture for his 1923 Nobel Prize in Physiology or Medicine, insulin is not a cure.
As a result, a major thrust of the scientific symposium focused on the innovative scientific research that will hopefully one day relegate a disease that affects 420 million globally to the dustbin of history.
Daniel Drucker and Gillian Hawker, both professors in the department of medicine in U of T’s Temerty Faculty of Medicine, kicked off the scientific symposium by moderating a panel with scientists from three major pharmaceutical companies engaged in diabetes research.
“What we are really looking forward to is to apply the powerful science that has become evident in the last few years to move beyond insulin toward a cure,” said Drucker, who is also a senior investigator at the Lunenfeld-Tanenbaum Research Institute at Sinai Health and a recent recipient of the Canada Gairdner International Award.
“How are your companies going to potentially cure diabetes?”
The scientists – from Eli Lilly and Company, Novo Nordisk and Sanofi – proposed stem cell-based approaches and immunotherapies that are in their early stages of development. They also raised the possibility of screening and preventing type 1 diabetes before it manifests as a way to substantially reduce the incidences of disease.
In the nearer term, conference attendees also spoke about the need to improve access to affordable insulin and other treatments for diabetes patients around the world, including in wealthy countries like the U.S.
“That’s unforgiveable, to have people take a suboptimal dose of insulin because they can’t afford the therapeutic dose,” Bernard Zinman, a professor in U of T’s department of medicine and a senior scientist at the Lunenfeld-Tanenbaum Research Institute, told symposium attendees.
Experts also noted that, because insulin is temperature-sensitive and has a short shelf life, maintaining supply in remote regions is particularly difficult. It can also be challenging to make new devices and other therapies available to resource-limited parts of the world, they said.
“The burdens and opportunities are different from country to country for people with diabetes,” said Dana Lewis, an insulin-dependent diabetic and University of Alabama alumna who created an open-source artificial pancreas system that automates micro-adjustments of insulin delivery to the body.
The issue of equitable access was addressed in a presentation by Jean Claude Mbanya, a professor of medicine and endocrinology at the University of Yaoundé I in Cameroon. Mbanya outlined how the absence of government policies, mark-ups in the supply chain and the organization of diabetes management within health-care systems can all impact patient access to insulin.
John Buse, the Verne S. Caviness Distinguished Professor at the University of North Carolina School of Medicine, gave a presentation on the future of insulin management in type 2 diabetes. He pointed out that while insulin has higher efficacy than many of the alternative drugs now available for type 2 diabetes, it has also been associated with weight gain and hypoglycemia (low blood sugar).
“The landscape has changed, and insulin has gone from being the only therapy available for type 2 diabetes beyond lifestyle management, to one that has advantages and disadvantages,” said Buse, who directs the diabetes centre at his university and who won the 2019 American Diabetes Association Outstanding Achievement in Clinical Diabetes Research Award.
Other approaches, including GLP-1 therapies, have comparable efficacy to basal insulin without the same adverse effect of hypoglycemia, Buse said, declaring it a “tie” between the two treatments.
“Insulin therapy is often necessary, but rarely preferred in the setting of type 2 diabetes due to weight gain, hypoglycemia, general complexity of initiating and titrating therapy, and lack of clear-cut cardiovascular benefits,” he said.

James Shapiro, a professor at University of Alberta who was the first in Canada to start clinical trials with human embryonic-derived insulin-producing stem cell transplants, spoke on the future of pancreas and islet transplantation.
“Islet transplant has the capacity to cure diabetes,” Shapiro said.
Shapiro added, however, that the approach is currently limited by the number of cells that can be acquired from an organ donor and risks linked to the anti-rejection drugs required for a transplant –challenges he’s working on solving with other scientists and biotechnology companies.
“This is my firm belief: diabetes will become a thing of the past if all goes according to plan,” he said.
In addition to the work of leading scientists in the field, the scientific symposium also recognized the work of trainees and early-career researchers who are making significant contributions to diabetes scholarship.
Awards were given to graduate students, post-doctoral researchers and early-career researchers studying diabetes. They included: Imperial College of London’s Steven Millership, Rebecca Cheung and Grazia Pizza; McMaster University’s Marie Pigeyre; Aviroop Biswas, an assistant professor at U of T’s Dalla Lana School of Public Health; and Saad Khan, a U of T doctoral student in immunology who studies links among the immune system, inflammation and obesity in metabolic diseases.
Drucker ended the symposium on a hopeful note by calling for a day when insulin therapy is no longer needed.
“The science that I heard in the last two days gives me tremendous optimism,” he said. “Let’s try to eliminate type 1 diabetes, so there is no 125th anniversary.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Rich culture and resilience: Reflections on Operation Remote Immunity
A group of Temerty Medicine residents and faculty members are among the health professionals travelling to remote Indigenous communities to provide COVID-19 vaccines as part of Operation Remote Immunity.
The plan was co-developed by Nishnawbe Aski Nation (NAN), which represents 49 First Nation communities across northern Ontario, and, which provides air ambulance and critical care transportation. During the initiative, vaccination teams will travel to 31 fly-in NAN communities. The goal is to complete Operation Remote Immunity by the end of this month.
A dozen resident and faculty physicians from Temerty Medicine were selected to take part in Operation Remote Immunity, which attracted an overwhelming amount of interest from potential volunteers.
The group included three Indigenous physicians from the Temerty Mecdicine community, Lisa Richardson a professor of medicine, Indigenous health lead for the Department of Family and Community Medicine Suzanne Shoush and fourth-year paediatrics resident Dr. Ryan Giroux, to support the teams’ learning and model culturally safe care provision.
“What was most inspiring for me was the leadership of the FN communities. Ornge provided the technical service and medical expertise in partnership with the communities, a true example of collaboration to support self-determination,” says Richardson, who is also strategic advisor in Indigenous health, vice-chair of culture and inclusion in the Department of Medicine and an internist at University Health Network and Women’s College Hospital.
“In remote communities, accessing specialized medical care means flying to larger centres. This may result in the introduction of COVID-19 and compromise access to care,” says Jillian Baker, a paediatrics professor. “COVID-19 in Indigenous communities could be devastating, and I wanted help provide these deserving communities an opportunity for primary prevention against it.”
Baker, who is also a pediatrician and pediatric/young adult hematologist at Unity Health Toronto spent a week in Pikangikum First Nation to assist with the vaccination efforts. Family medicine residents Drs. Kate MacNaughton and Elliot Lass were also part of the group that travelled to Pikangikum, which is about 300 kilometres northeast of Winnipeg. MacNaughton has a focus on global health and vulnerable populations and Lass is specializing in care of the elderly.
Drs. Shima Shakory, a first-year resident in family medicine and public health and preventive medicine and Jonathan Kwong, a second-year emergency medicine resident both spent a week in Sandy Lake, about a 45-minute flight from Sioux Lookout.
Recently, the group shared some of their reflections with writer Erin Howe.
What was it like to work in Pikangikum?

MacNaughton: Pikangikum is a special place to work: its population is about 3000, many community members are young and Ojibwe remains the first language for most residents. There are also challenges related to implementing a vaccination program including a lack of access to transportation and historically low rates of vaccination. In addition, people face ongoing injustices that contribute to ambivalence toward outside health programs.
Our group was joined by an Independent First Nations Alliance (IFNA) team and by local members of the Canadian Rangers — their involvement was crucial to the initiative’s success. We worked in small interdisciplinary teams, conducting home visits to answer questions and to provide vaccines to people who were homebound for various reasons. These visits were a wonderful opportunity to get to know the people and the community better.
My IFNA and Canadian Ranger colleagues were respectful and friendly. Our teams were united and motivated and we exceeded local expectations for vaccine uptake.
Taking our constructive interactions as a matter of course illustrates my privilege as a non-indigenous person living in Canada. After all, if one of my indigenous co-workers presented to a hospital in Ontario, would they have had the same implicit presumptions of fair and unbiased treatment from our health care system?
What did you do to ensure you were providing culturally safe, culturally sensitive care?

Lass: Before we left for Pikangikum, our team participated in the San’yas Indigenous Cultural Safety Training Program. The course taught us about their history and traditions and the moral imperative to ensure that they were vaccinated in a safe and effective manner.
One of the first people I met while in Pikangikum was Dean, an educator and community leader. He manages the community Facebook group which almost every adult in Pikangikum follows. We decided to do a live Q&A about the COVID Vaccine which helped us virtually interact with the broader community.
I built a great relationship with Dean and am in awe of his tireless work. He visited the vaccine site daily and inspired his community to get vaccinated. On our last day, we even did a mask exchange — we gave him a University of Toronto mask and he gave us a Pikangikum mask. It was symbolic of the connection we made on our shared mission.
Spending the week in Pikangikum helped me learn more about the resilience of the Indigenous people. This experience has inspired me to go back to indigenous communities in the future as a family physician.
What were some of the highlights of this experience?

Baker: It was a wonderful experience to be invited into people’s homes, hear their stories and learn from them.
Working with the young local Rangers in the community was a highlight for me, as well as the interactions with community leaders who were welcoming and dedicated to ensuring every member of their community had access to the vaccine.
Having learned about the suppression of the First Nations languages and culture, I was heartened to hear Ojibwe shared across generations, from the elders to the youth. I was impressed by the community’s pride and the spirit of perseverance in Pikangikum.
What was it like to work with local leadership in Sandy Lake?
Shakory: The community had amazing local leadership. Months before any vaccine approval, they started building vaccine confidence by discussing safety and efficacy over the radio. They advertised the mass vaccination clinic before and during the campaign using Facebook Live and the radio. The Oji-Cree community is home to about 3,000 people, including nearly 1,350 vaccine-eligible adults.
The local team set up the mass vaccination clinic before our arrival, with best public health practices in mind. There were nine vaccination stations, distanced across the elementary school’s gymnasium. When clients entered the clinic, they met greeters and screeners. Runners guided clients to the vaccination stations, where we immunized them. Once vaccinated, clients were walked to the waiting area. After waiting 15 minutes, they exited, following a one-way flow. The clinic functioned smoothly thanks to the Sandy Lake community and Ornge leadership.
Reflecting on our experiences, our team was inspired by the communities, and we would each be honoured to return in the future.
Are there any interactions that had a particularly big impact on you?
Kwong: I previously spent a few weeks volunteering in Pond Inlet, Nunavut and jumped at the opportunity to learn more and to do the meaningful work of providing vaccinations.
One interaction that stands out to me took place during a home visit to vaccinate a community member with limited mobility who was unable to attend the vaccination clinic. When I entered the house, I saw what could be described as impoverished living conditions. Having seen similar conditions in Nunavut, I was reminded of the systemic causes of such striking inequity in Canada, the disadvantages Indigenous communities face and the privileges we have living in Southern Ontario.
Before we vaccinated the community member, their family requested a smudging ceremony to pray for their loved one’s safety and that of their community. It was a privilege to be part of such an intimate, traditional ceremony. After the vaccine was given, we bonded over childhood memories and family pictures. I left feeling I’d learned some beautiful lessons about the family and their culture.
Although I initially thought this experience would prompt me to reflect on my own privilege and the inequities facing Indigenous communities, I was also inspired to learn more about their rich culture and the resilience.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Remaining Committed Until The End
More than a year into the COVID-19 pandemic, we mark another Passover, Easter, and Ramadan celebrated under a lockdown. Another return to virtual classes for children. Another birthday missed or milestone canceled. It’s easy to understand the frustration and the desire to return to things as they once were. Yet, for those on the frontlines fighting this pandemic, the challenges have only grown, and the cost of complacency has become evident.
It’s clear the third wave of this pandemic is nothing like what we’ve seen before. The new variants are spreading faster and causing greater illness. The rates of infection are growing exponentially, especially among younger age groups. As a result, our healthcare system is facing unprecedented strain. And, in turn, this has placed unparalleled demands on healthcare workers. This includes canceling elective surgeries and redeploying staff to critical frontline units.
This happens as we can envision a time when everyone is vaccinated. In a marvel of scientific discovery, we have seen vaccines developed with incredible efficiency. Ensuring they reach those in greatest need has to be a top priority. That’s one of the reasons I am proud of the University of Toronto’s efforts, supported by many in our Faculty, to open and operate vaccine clinics. We must also use our knowledge and positions to educate our communities about the effectiveness of vaccines to overcome hesitancy. While there have been reports about potential side-effects associated with certain vaccines, they remain overwhelmingly safe, and the concerns expressed by regulators demonstrate the rigorousness and seriousness of the protocols that ensure patient safety.
We must also be effective advocates for our patients and communities while we strive towards the finish line of this pandemic and beyond. So many in our Faculty have responded to this need – learners, staff, faculty and researchers alike. I am thankful for those who, in addition to carrying the heavy burden of delivering care, are making the needs of their patients known to policymakers and the public at large. In addition to their physical health, we must also be concerned for their mental health as well as their economic, social and cultural safety.
Ending this pandemic is achievable because we have the necessary tools and knowledge. I have also seen the effort, dedication and sacrifice made by members of the Temerty Faculty of Medicine and at all of our partner institutions. Your work has had a considerable impact on fighting this virus and delivering the care that is so desperately needed. I want to thank you for all that you have done – and will do. Only together will we prevail.
Trevor Young
Dean, Temerty Faculty of Medicine
Vice Provost, Relations with Health Care Institutions
P.S. Please continue to look out for your own wellness and the wellbeing of your colleagues. A list of resources is provided below.
Wellness Resources
Learners
Office of Health Professions Student Affairs (for MD Program, MD/PhD, Medical Radiation Sciences, Physician Assistant, and Occupational Therapy students)
Postgraduate Wellness Office (for Post MD learners)
Student Health and Wellness (for graduate students)
U of T My Student Support Program (My SSP) | 1-844-451-9700. Outside of North America, call 001-416-380-6578.
Culturally-competent mental health and counseling services in 146 languages for all U of T students.
Good2Talk Student Helpline | 1-866-925-5454
Professional counseling, information and referrals helpline for mental health, addictions and student well-being.< /p>
PARO 24 Hour Helpline | 1-866-HELP-DOC (1-866-435-7362)
The PARO 24 Hour Helpline is available to residents, their partners and family members, as well as medical students.
Faculty
Wellness Resources for Faculty
Staff

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Giving Back: Retired Faculty Member Endows New OBGYN Professorship
Dr. Samuel Librach (MD’52), may never have known his grandmothers during their lifetimes, but he credits them for helping inspire his trailblazing career in obstetrics and gynaecology.
“Both my mother’s mother and father’s mother died during, or as a direct result of, childbirth,” he says. “Care in the small towns in Poland in which they lived at that time simply wasn’t well-developed. While I always wanted to pursue medicine, I think my grandmothers’ experiences definitely shaped my decision to work in this field.”
It’s no surprise then that, when reflecting on his more than five decades as one of Toronto’s leading obstetricians and gynaecologists and University of Toronto professor, Samuel is most proud of the role he played in preventing maternal deaths.
“I was chief of service for obstetrics and gynaecology at The Doctor’s Hospital for more than 19 years. During that time, not a single woman died in childbirth. We had deaths before, and the hospital had them after — but there was not one under my care.”
When asked about Samuel’s impact on their shared field, his son, Dr. Clifford Librach (MD’83) is quick to point out his father’s track record of innovation and dedication as a medical educator.
According to Clifford, who followed in his dad’s footsteps and now serves as a professor of reproductive endocrinology and infertility at U of T, Samuel helped develop a specialized laparoscopic instrument and also pioneered the use of the now-standard Pfannenstiel incision (or “bikini cut”) for caesarean section births in Toronto.
“My dad was such a talented gynecologic surgeon — probably one of the best in the entire city when he practiced — and a gifted teacher,” Clifford says. “It was a testament to him and his skill that he was the one colleagues would call in when they had a particularly challenging case. When you were in trouble, your first call was to Sam Librach for help.”
Now, true to that spirit of innovation and commitment to helping his peers, Samuel and his wife Evelyn have made a generous gift to the University to establish a new Early-Career Professorship in Obstetrics and Gynaecology named in their honour.
“While my dad was a clinician through and through, he thinks research is amazing and can see its benefit on future generations of practitioners,” says Clifford. “This new endowment will help develop new clinician-scientists just starting off in the field, ensuring they have the resources and support they need to launch successful careers.”
Clifford also notes the importance of the fund’s name in recognizing his mother’s central role in his father’s work.
“My mom gave up her own university and career ambitions to support my dad during his training,” he says. “When he was a resident, earning hardly anything, she worked two jobs selling jewelry and bookkeeping. Later, she completed her Bachelor of Arts at U of T and put her natural business skills to work by investing in real estate. She’s a big part of why he was able to have the career he did, and why they are able to make this gift today.”
Samuel also sees their contribution as a way for his career to come full circle — giving back to the institution where he had his start.
“When I was a student at the University of Toronto, I received money for a bursary,” he says. “It was several thousand dollars and was a big help. I always thought someday I like to give back to U of T and I guess this is a good time to do so.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
