IGNITE to Empower Future MD Students
The MD Program’s Community of Support (CoS) will welcome nearly 300 aspiring physicians when it hosts its second annual IGNITE Conference this Saturday at the University of Toronto. The event will also mark an exciting milestone for the 3-year old CoS network— some talks will be delivered by current MD students who benefitted from the CoS program.
CoS works to increase the number of medical students who are Black, Indigenous, Filipino or economically disadvantaged. It helps link students from these underrepresented communities to volunteer opportunities, Biostats enrichment courses, the MCAT Student Support Program and application support for students applying to medical school or for research positions. The program also offers mentorship by medical students and doctors at various stages of their training and careers.
“The conference really crystalizes the resources CoS links students to” says Ike Okafor, Senior Officer, Service Learning and Diversity Outreach in the Faculty of Medicine’s MD program.
The conference content was developed in consultation with CoS members and current physicians who understand the intricacies of the application process and the rigours of medical school training.
There are now more than 1,000 CoS members and a dozen student-led chapters across the province and beyond. For example, teams at Ottawa, Western, U of T, Queen’s University and McMaster performed mock interviews with CoS members to help candidates prepare for their medical school interviews, a critical step in a rigorous process. As well, at an administrative level, Okafor collaborates with colleagues at other medical schools including McGill, Dalhousie and Harvard to obtain student support in the application process.
The conference will feature talks about the Ontario Medical School Application Service (OMSAS), the Medical College Admissions Test (MCAT), tips for interviews and securing references and information about admissions to medical schools in the United States and Caribbean.
“We want to help eliminate barriers and support students in pursuing their goal to attend medical school, regardless of where they end up applying,” says Okafor. “We’ve been able to help students who have accepted offers from medical schools across North America.”
Aspiring medical students will have the opportunity to meet MDs who embody their dreams. Participants will also be able to connect with current medical students, admissions staff and community organizations. The day-long event will also provide a chance for students to network with physicians working in a variety of specialities.
“There is a thriving community of physicians of Afro-Caribbean and Indigenous descents,” says Dr. Renée Beach, dermatologist and outreach lead for the Black Physicians’ Association of Ontario. “A lot of the time we’re working hard seeing patients and doing research, but it’s really important for us to take some time to connect with who we hope will become the future generation of physicians.”
Listen to Dr. Beach on CBC’s Metro Morning
Last year’s conference attracted about 200 participants. Attendance at this year’s event is expected to be even higher, with students from as far as Ottawa and London planning to attend.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Faces of U of T Medicine: Dr. Neil Isaac

Early in his education, Dr. Neil Isaac developed a passion for science. In addition to being an adjunct lecturer in the Department of Medical Imaging, Isaac is also a general radiologist at North York General Hospital and is working to increase the representation of Black students in medicine through his role with the Black Physicians' Association of Ontario (BPAO). As U of T Medicine celebrates Black History Month, writer Erin Howe asked Isaac about his work and advice for Black students who want to follow in his footsteps.
What sparked your interest in medicine?
I’ve always been always interested in the sciences. I found them interesting and liked that if you had the answer, you were correct — there are no shades of grey, no interpretative errors. I also liked the impartiality of grading those courses! I trusted that if I knew my stuff, there would be no bias in marking, no weighing past tests into my mark. The answer was the answer.
The quest for the answer is what led me into what I would consider the ultimate career for people who like to answer questions (other than scientist) — for me that was medicine.
Can you tell me more about your work as a radiologist?
I’m fellowship-trained in cardiovascular imaging, but I like keeping on top of what’s new and interesting in radiology and don’t like to pigeonhole myself into any one area. As such, I can enjoy freedom of movement should I wish to leave my department (I won’t!) as well as some job security, because I’m not stuck in one particular area, where a paradigm shift might render that area useless — like pneumoencephalograms, a type of head x-ray that’s been replaced by MRI and CT scans.
What do you find most exciting about this area of medicine?
The constant evolution and innovation. Every year, there is a humongous conference in Chicago where radiologists, physicists, technologists, nurses and our industry partners get together to showcase the latest and greatest in radiology and to exchange ideas. It’s a very exciting conference that I try to get to as often as possible.
You’re also on the board of the BPAO — what do you enjoy most about being involved in this organization?
I look at it as an opportunity to give back. I have been quite fortunate to make it where I am today. But I must recognize those that have come before me. I can count on two hands the number of Black radiologists in Ontario. Black people, and several other racialized minorities, are underrepresented in medicine. For some people, being seen by someone with a shared experience — like their country of origin, religion or race— really helps in their therapeutic bond, or willingness to seek out help.
What advice would you offer to Black students interested in pursuing a career in medicine?
Work hard. Always push for your goal. It will be tough, and there will be many people discouraging you. But there will also be others encouraging you. Look to them. Block out the negative. Surround yourself with positive people and like-minded individuals who are also striving to fulfill their dreams.
Faces of U of T Medicine introduces you to some of the interesting people studying in the Faculty of Medicine. From advising political leaders to providing care to Toronto’s most vulnerable populations, members of our community are having an impact at home and around the world.
Do you have an interesting story to share? Contact us at medicine.communications@utoronto.ca.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Environment More Important to Respiratory Health Than Genetics: U of T Researcher
A University of Toronto researcher has found strong evidence that environmental exposures, including air pollution, affect gene expressions associated with respiratory diseases much more than genetic ancestry.

Senior author Philip Awadalla, a professor in the Department of Molecular Genetics, analyzed more than 1.6 million data points from biological specimens, health questionnaires and environmental datasets. His study is one of the largest ever to examine the relationship between gene expression and environmental stimuli.
His findings, published March 6 in Nature Communications, represent a groundbreaking use of big data to uncover the environmental factors that are behind diseases and inform strategies for prevention, an approach that would apply to a number of diseases, including cancer.
“Our study shows how one can use the large scope and scale of data in Canada’s largest health cohort to better understand how our genes interact with environmental exposures and shape individual health,” says Awadalla. “I encourage all those engaged in this type of research, both in Canada and around the world, to take advantage of this resource.”
Genetic, health and disease data of participants from Montreal, Quebec City and Saguenay were linked with environmental information such as air pollution, walkability and access to food to see how these factors impact gene expression. Participants were enrolled in the Quebec arm (CARTaGENE) of the Canadian Partnership for Tomorrow Project (CPTP), which supports research into environmental, lifestyle and genetic factors related to the development and progression of cancer and chronic diseases. More than 300,000 Canadians, one per cent of the population, have enrolled in CPTP since its launch in 2008.
The study used deep characterization of gene expression signatures from participants and linked that data with environmental information. “We were surprised to find that we were able to stratify genetic ancestry within Quebec, identifying individuals whose descendants were from Montreal versus Saguenay for example,” explains Awadalla, who is also Sr. Principal Investigator, Computational Biology, for the Ontario Institute for Cancer Research. “This helped us to show how most gene expression is not derived by ancestry, and that environmental exposures associated with living in a particular city or region are more impactful on gene expression associated with disease traits than heritable variation.”
One of the main findings of the study was that exposure to higher levels of particulate matter and nitrous dioxide in the Saguenay area affected the expression of genes associated with oxygen pathways and respiratory function. This resulted in higher rates of respiratory ailments such as asthma and chronic obstructive pulmonary disease (COPD). The study also revealed that there are genetic variants that control how a person’s gene expression responds when exposed to environmental stimuli.
Controlled access to cohort data and biological samples is available to researchers through the CPTP Data Portal and CARTaGENE.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

U of T Professors Lead Lancet Special Report on Canadian Health Care
The Canadian government must match its public declarations with concrete action on issues such as disparities between Indigenous and non-Indigenous peoples’ health, health system reform, and flagging levels of overseas aid, if it is to renew its legacy of leadership in health, according to a new issue of The Lancet examining Canada’s system of universal health coverage and role in global health.
 The lead authors of the two commissioned papers are Danielle Martin, Associate Professor of Family and Community Medicine, and Stephanie Nixon, Professor of Physical Therapy, both at the University of Toronto. Co-authors include leading scholars from across Canada.
The lead authors of the two commissioned papers are Danielle Martin, Associate Professor of Family and Community Medicine, and Stephanie Nixon, Professor of Physical Therapy, both at the University of Toronto. Co-authors include leading scholars from across Canada.
Martin and her co-authors argue that reform is needed for Canada’s universal health care system to recommit to and deliver on its founding principles of equity, solidarity, and co-stewardship.
While urgent medical and surgical care is generally timely and of high quality, wait times for elective care have been a lightning rod. One in three Canadians must wait more than two months for a specialist referral, far higher than many OECD countries. Canada also faces an ageing population, growing multiculturalism and urbanisation, and a geographical vastness that makes the delivery of health care to rural and remote communities especially challenging.
“Medicare is a source of national pride and a model for achieving universal health coverage, but without reform, the system risks becoming outdated,” writes Martin, who is also Vice-President, Medical Affairs and Health Systems Solutions at Toronto’s Women’s College Hospital. “Rather than continue the Canadian tradition of slow, steady, and incremental change, Canada needs to step forward boldly to ensure a vital and sustainable health system for all Canadians. Provincial and territorial governments cannot succeed alone; the federal government now needs to renew its national vision for health care, recommitting to core Canadian values of equity and solidarity.”
Similarly, on the global stage, the authors call for bold, strategic action to realise its vision of being a progressive force for health. Canada has a long history of strong engagement and leadership in global health, leveraging its assets as a middle power to build consensus and advance health equity.
Over time, Canada’s development assistance for health (DAH) increased more than seven times between 1997 and 2016, up to 2.5 per cent of the world’s DAH, mostly through multilateral channels. However, overall overseas development aid has declined, with Canada’s contribution standing at just 0.26 of GDP, placing it 15th among 29 OECD countries, well below the 0.40% OECD average, and the UN target of 0.7%.
“Prime Minister Trudeau’s progressive statements about immigration, gender equality, and climate change are welcomed, and have created expectations about elevated Canadian leadership on the world stage,” writes Nixon, an HIV expert who is also director of U of T’s International Centre for Disability and Rehabilitation. “But now is the time to match words with government actions.”
The analysis is accompanied by commentaries from Prime Minister Justin Trudeau and Jane Philpott, Minister for Indigenous Services, who lay out Canada’s vision for global health and gender equality, along with the country’s plans to improve Indigenous health and wellbeing.
Writing about Canada’s new Feminist International Assistance Policy, Prime Minister Trudeau says: “Our goal is to enable and empower women and girls so that they can reach their full potential. Canada cannot create this change alone. But we can accomplish a great deal when we come together. In June, 2018, Canada will host the 2018 G7 Leaders’ Summit where gender equality will be at the top of the agenda.”
Philpott writes: “The historical denial of the rights of Indigenous peoples is directly linked to socioeconomic disparities, including poor health outcomes… Correcting for these inequities requires more than better health care. Health-care workers who respect Indigenous knowledge and practices are vitally needed and health-care systems must be improved. But real change requires the recognition of the inherent and treaty rights of Indigenous peoples, along with investments in the social determinants of health.”
The issue was launched on February 23 in Ottawa.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

On Being a Black Woman in Medicine
They told her step back/they asked for credentials/ I do not have my credentials but this man’s vitals are waning/they told her step back/how can you be both doctor and black?/I ask myself the same.
--from "Woman, Black" by Chika Stacy Oriuwa
The U.S. border agent looked at Chika Stacy Oriuwa and refused to believe she was training to become a physician. “He accused me of lying and said ‘I doubt you’re going to do that,’” recalls the second-year U of T medical student.

Patients, too, have sometimes needed convincing that Oriuwa, a Black woman, is in fact a medical student and not a technician or nurse’s aide.
Then there was the case last year of the African-American physician, Dr. Tamika Cross, who was prevented from helping a patient in distress because a flight attendant didn’t believe she was a doctor. Inspired by that incident, and to combat the discrimination she experiences in medicine, Oriuwa earlier last year wrote a poem, "Woman, Black," and posted a YouTube video of herself reciting it.
“The poem aims to explore the intersectionality of race, medicine and gender, specifically my narrative of medicine, being the only Black woman in my class, facing the racism and sexism in my institution,” says Oriuwa. “But it’s a commentary on all medical schools. They need to do a better of job in helping us to navigate the discrimination we’ll face as physicians.”
So far, says Oriuwa, “I’ve received pretty great responses to the video. It’s great to know that this issue is something a lot of other people are dealing with. It just hasn’t been brought to the forefront yet. We are expected to learn how to deal with discrimination in the workplace -- there’s no formal guidance on how to deal with these situations and mitigate the emotions.”
The video has been seen more than 3,000 times on Youtube, and Oriuwa was also featured in Flare magazine.
Faculty of Medicine leaders agree that more should be done to prepare learners for discrimination on the job.
"The faculty of medicine has made a lot of progress over the last few years, incorporating topics like racism, privilege, and allyship into the medical curriculum,” says Professor Onye Nnorom, Black Health Theme Lead in the MD Program. “However, more needs to be done to ensure that we are protecting our students, particularly those who come from historically disadvantaged groups, from both macro- and micro-aggressions that could adversely affect their success and their wellness.”
The Faculty has also begun surveying residents about their well-being, including whether they have experienced discrimination or harassment, and plans are in the works to extend the survey to other learners at the Faculty of Medicine. The data should help the Faculty to develop curricular and extra-curricular ways of addressing the reported problems.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Heidi Singer

Personal Genome Project: First Results Are In
Researchers from The Hospital for Sick Children (SickKids) and the University of Toronto behind the Personal Genome Project Canada (PGP-C) are predicting whole genome sequencing will likely become part of mainstream health care in the foreseeable future.

In the first-ever study from PGP-C, the researchers found 25 per cent of participants to date had genomic information indicating they could be at risk for future disease and even more were found to have genetic variants that would be relevant for family planning or newborn screening. All participants had genomic information associated with risks for adverse drug reactions or altered drug effectiveness, with 23 per cent of participants identified as being at risk for severe, potentially life-threatening adverse drug reactions. The study was published Feb. 3, 2018 online in CMAJ (Canadian Medical Association Journal).
PGP-C is a comprehensive public data resource that integrates participants’ whole genome sequencing data with their health information to advance scientific understanding of genetic and environmental contributions to human health and disease. All of the Project’s inaugural 56 participants have clinically relevant information in their genomes, highlighting the potential of using whole genome sequencing data proactively for precision medicine and to reduce the risk of therapeutic failure.
“Though we’ve identified clinically relevant genomic information for all participants, each of their genomes has even more information that we can’t interpret yet,” says Stephen Scherer, Director of U of T's McLaughlin Centre and Senior Scientist and Director of The Centre for Applied Genomics (TCAG) at SickKids. “As we analyze more samples, we continuously learn more about the human genome which will allow us to eventually take full advantage of the wealth of information it contains. That’s why the goal of the Project is to sequence thousands of genomes each year.”
PGP-C is the Canadian arm of the global Personal Genome Project, a collaborative academic research effort that started with Harvard Medical School’s Personal Genome Project in 2005. A priority of the Personal Genome Project is to share information collected from the localized projects with researchers around the world to drive new knowledge about human biology.
Participants were required to undergo an extensive consent process as all data, including results from their whole genome sequencing, combined with personal and family history, is available online. Each participant had access to genetic counselling to appropriately contextualize the results of their genetic testing.
“Genetic counsellors play an important role in communicating and interpreting these results appropriately,” said Professor Trevor Young, Dean of the Faculty of Medicine at the University of Toronto, which runs Ontario’s only academic training program for genetic counselling. “The demand for these specialized skills is only going to rise given the massive increase in the number of genome-wide tests now being used in hospitals.”
The cost of whole genome sequencing has fallen dramatically since PGP-C began recruiting and analyzing samples in 2012 and further still from when the Project was conceptualized in 2007. Signs indicate the technology will continue to become more affordable and accessible, which the authors expect will transform whole genome sequencing into more of a mainstream practice for the general population. As a result, frontline health-care providers may become involved in interpreting and delivering resulting genomic information in the near future.
The work was funded by the McLaughlin Centre, the Canada Foundation for Innovation, Genome Canada/Ontario Genomics, the Government of Ontario, the Canadian Institutes of Health Research (CIHR), Medcan Health Management Inc. and SickKids Foundation.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

U of T Scientists Create Mirror-image Molecules to Develop Better Medicines
 U of T researchers have developed a new technology for creating more durable disease-fighting molecules which could lead to drugs with longer-lasting effects.
U of T researchers have developed a new technology for creating more durable disease-fighting molecules which could lead to drugs with longer-lasting effects.
The technology involves the creation of mirror-image versions of existing drugs, which last longer in the body because they’re harder to digest. For patients, this would mean less frequent drug injections and more medicines could potentially be made available as pills.
But designing these drugs has always been tricky.
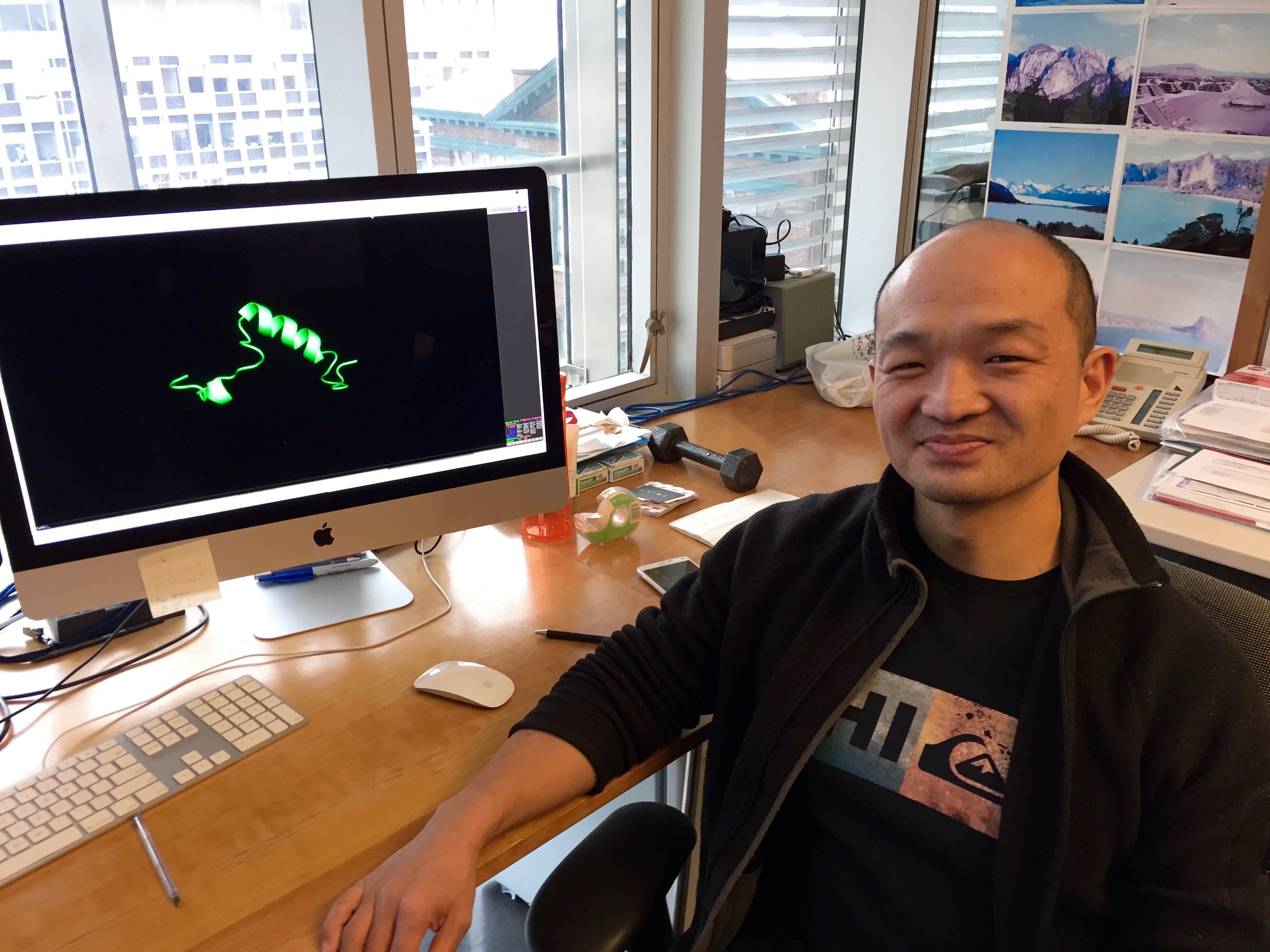
Now a team of researchers led by Philip Kim, a professor of computer science and molecular genetics in the Donnelly Centre for Cellular and Biomolecular Research, has developed a new technology for making mirror-image peptides, which bind and activate receptors on the surface of cells. They created mirror-image versions of two blockbuster drugs, a diabetes medication called glycogen-like-peptide 1 (GLP1) and the thyroid drug parathyroid hormone (PTH).. In studies, both mirror-image counterparts had longer effects on cells than the existing drugs.
The findings are described in the January 29 early online edition of the Proceedings of the National Academy of Sciences.
“Mirror image peptides are not recognized and degraded by enzymes in the stomach or bloodstream and therefore have a long-lasting effect,” says Kim. The other advantage, he said, is that mirror-image peptides also get overlooked by the immune system, which often mistakes natural peptides for foreign invaders and thus limits drug efficacy.
Peptides are made from molecules called amino acids. For reasons that are not fully understood and which go back to the origin of life, almost all amino acids in the natural world occur in one geometric form. Their atoms are arranged in such a way that makes the entire amino acid molecule appear left-handed, or "L" for short. As a result, natural peptides are also left-handed. Because peptides produced by microbes, plants and animals can be harmful, the human body has evolved efficient ways to purge them.
But if you inverse a peptide, by making a mirror-image of it, it can still bind correct receptors while sliding unnoticed past the body’s defense mechanisms. Mirror image peptides can be made in the lab from synthetic right-handed amino acids, which are also known as “D” for dextrorotary.
Unlike straight L peptides, which can be fairly easily converted to a D form, most biologically active peptides are twisted into helices, and so far there has been no good way to design their mirror-image counterparts on a large scale, said Kim.
Using a purely computational approach, Kim’s team was able to clear this obstacle. They started with the largest public database which contains structural information for three million helical peptides. They then created an algorithm to flip these peptides into their D versions. Finally, the team looked in this new virtual library of mirror-image peptides for those that best matched GLP1 and PTH.
Once they found the match, the researchers had the D-peptides synthesized and tested for their ability to activate their receptors on the cell’s surface. They found that both D-GLP1 and D-PTH elicited cellular responses similar to their natural counterparts but had a longer-lasting effect.
“We are now investigating whether the D-PTH could be orally delivered because it is avoiding breakdown in the stomach”, says Kim. “For frequently dosed medication, this is of great interest, as taking a pill is much easier than having an injection. This could lead to many more peptide drugs being taken as pills”.
Currently, patients who take GLP1, which was discovered at U of T by Professor Daniel Drucker, of the Department of Medicine, or PTH, must inject these drugs on a daily basis.
Kim is working with the U of T patent office to protect his technology as he explores opportunities to partner with the pharmaceutical industry to commercialize the research. He is also developing mirror-image versions of peptides that work against the Dengue and Zika viruses in order to make them more durable in the bloodstream.
“We are testing our approach on as many interesting peptides as we can,” Kim said.
The study was funded by research grants from the Canadian Institute of Health Research and the National Sciences and Engineering Research Council of Canada.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Jovana Drinjakovic

New Bright Angel for Developing Antifungal Drugs
Dr. Luke Whitesell, the company’s co-founder and scientific advisor, recently relocated to Toronto from Cambridge, Massachusetts, where he helped lead research in the large, interdisciplinary Lindquist Lab at the Whitehead Institute for Biomedical Research, which is affiliated with the Massachusetts Institute of Technology (MIT). Previously, Whitesell had his own lab at the University of Arizona, where he was a professor of Paediatrics. He has also collaborated with a variety of research groups including teams at the MIT Koch Institute for Integrative Cancer Research, Harvard Medical School’s Institute of Chemistry and Cell Biology and the National Institutes of Health National Centre for Advancing Translational Sciences to find new therapeutics through chemical screening projects.
In addition to his new role with Bright Angel, Whitesell is also a senior research associate in the lab of Professor Leah Cowen, Chair of the Department of Molecular Genetics. He recently spoke to writer Erin Howe about his research and new role.
Tell me about Bright Angel’s goals — I understand the company is working to develop a drug that will help fight drug-resistant fungal diseases.
Launch of the company was made possible by partnering with Schrödinger, Inc., a privately-held company dedicated to revolutionizing drug discovery through advanced computational methods, and MaRS Innovation, a non-profit organization supporting the commercialization of research breakthroughs from Toronto’s leading academic institutions. The limited interest of large pharmaceutical companies in developing antibiotics is a well-recognized problem. The situation is concerning with regards to antibacterials, but far worse for antifungals where serious unmet medical needs not only persist, but are rapidly escalating. Given this challenging landscape, Bright Angel is pursuing a more cost-effective, biotech-based path to antifungal drug development made possible by new insights into the biology of fungal infections from the labs with which I have been involved and the engagement of Schrödinger and MaRS Innovation in the process.
What excites you most about this area of study?
Life-threatening infections by fungi have a huge impact on human health. These organisms pose a threat on par with prominent bacterial and protozoan pathogens such as those causing tuberculosis and malaria. The most vulnerable are people with compromised immune systems, including those undergoing chemotherapy, recipients of solid organ or hematopoietic stem cell transplants and those infected with HIV. In my former life as a paediatric oncologist, I saw many children die from uncontrollable fungal infections even though their cancer was under control. The opportunity to help provide much needed, better treatments for these kinds of infection is a very exciting prospect.
In addition to your work with Bright Angel, you’ve also been named a senior research associate in Professor Leah Cowen’s lab. What are you looking forward to in this part of your work?
I have known Professor Cowen for over a decade now, since she was a postdoc in the laboratory of Susan Lindquist when I was on a sabbatical from my position as professor in the College of Medicine at the University of Arizona. Because of our very different, but complementary areas of expertise, we have continued to work together over the years, especially in the area of heat shock biology. I know from personal experience she is a fantastic scientist. With my background in pharmacology and experimental therapeutics, I’m looking forward to helping her guide the drug discovery and chemical biology efforts being pursued by the great group of scientists she has assembled in her lab.
You’ve also practiced medicine as paediatric hematologist-oncologist. How does your clinical experience complement your work in the lab?
As a paediatric oncologist, I was involved in the clinical development of new cancer treatments for well over two decades and the care of many children with invasive fungal infections. I’m acutely aware of the need for better antifungal treatments and the specific gaps that need to be filled. I am convinced that new, more effective and resistance-disfavoring treatments can only be discovered and developed through a better understanding of the mechanisms by which fungi are able to infect people and grow within them. Deciphering these mechanisms is a major focus of the work going on in Professor Cowen’s lab.
What interested you in continuing your work at U of T?
come to the University of Toronto with the express purpose of helping Professor Cowen realize the challenging goals she has set for her research program and to help guide Bright Angel in these early days while it tries to turn theory into practice.
How are you settling in? What are your favourite parts of Toronto so far?
Our re-location to Toronto has gone surprisingly well. We were fortunate to find a nice, snug home to rent near the Christie Pits Park and Koreatown. I’m able to walk back and forth to the University, which allows me “thinking time” each day and provides for a bit of exploring along the way. We’ve enjoyed trying out the enormous variety of restaurants in our neighborhood. Our new neighbors have been very friendly and welcoming. The university administrators who facilitated my on-boarding have also been terrific.
As a bit of deep background, my 99-year-old mom is Canadian. She grew up in Medicine Hat, AB before being sent to the United States to work in the British Embassy during World War II, back when Canada was part of the British Empire. I spent many summers with my grandparents in Calgary and have done a lot of hiking, camping and fishing in the Canadian Rockies. My wife and I are looking forward to exploring the parks in Ontario, but only once it warms up a bit!

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

Faces of U of T Medicine: Maneesha Rajora
What’s the focus of your research?
My project focuses on the development of new nano- and micron-sized materials to deliver drugs to brain tumours. Currently, there’s no cure for glioblastomas, which are highly invasive brain tumours. One of the challenges is the blood-brain barrier (BBB), which prevents many drugs from reaching the brain and tumour cells. I’m trying to take advantage of properties unique to nano- and micron-sized particles to either bypass or transiently disrupt the BBB. This will allow me to enhance the delivery of otherwise impermeable drugs to brain tumours, ultimately opening the door to more therapeutic options for glioblastoma. Specifically, I’m trying to enhance the delivery of organic light-activated drugs called porphyrins, for targeted cancer phototherapy.
What interested you in pursuing this area of research?
During my undergraduate degree, I was drawn to the fields of synthetic and materials chemistry. I was enthralled by chemists’ abilities to apply fundamental scientific knowledge to create new molecules, materials and platforms that could impact the way diseases were treated and diagnosed. I really enjoy the creative design process and puzzle-solving that goes into materials development. The ability to engineer new materials from scratch that have potentially very real positive impacts on patients is extremely exciting!
What did receiving the Mr. Robert and Ms. Francine Ruggles Innovation Award mean to you?
This recognition was humbling and motivating. I’m surrounded by brilliant MD/PhD colleagues conducting impactful research. I was honoured to be chosen among such worthy candidates. Having trained in chemistry before entering the program, I have a traditionally unconventional research background and project. It was encouraging to see this diversity in research recognized, which I hope will reassure and motivate others pursuing their passion for biomedical research, regardless of their educational background or scientific discipline of interest.
What drew you to the MD/PhD program?
I was drawn to the quality of training I could receive through the U of T MD/PhD program as I pursued my goal of becoming a clinician-scientist. This ambition was shaped by my undergraduate and Master’s training. I did my undergraduate thesis project with clinician-scientist Professor Donald Weaver. His dedication to improving patient care through research and ability to navigate the space between clinical care and basic science sparked my interest in clinical medicine and inspired me to further pursue biomaterials research with Professor Paul Santerre for my Master’s degree. In the Santerre lab, I developed a passion for translational research and established my goal of combining this interest with practicing clinical medicine. The MD/PhD program is an ideal ground to explore my immediate scientific curiosity while staying in touch with the driving motivation of improving patient care. I saw, and continue to see, the MD/PhD program and a clinician-scientist career as a gratifying way of having a positive impact at an individual patient and family level, and more broadly to all patients affected by scientists’ biomedical interests.
What’s your favourite thing about the MD/PhD program?
The support within the MD/PhD program at U of T, whether its in the form of resources or people, is phenomenal. It grants trainees like myself with truly protected research time without being limited to field or time of study, which allows me to freely explore my scientific interests and get the most out of my PhD training. Most importantly, the program gives us a family of colleagues and mentors we can rely on for support through the ups and downs of what is a very dynamic and lengthy training program.
Where do you see yourself in 15 years?
The goal of becoming a clinician-scientist is alive and strong! In 15 years, I hope to be practicing as an academic clinician while leading a research team toward the development of materials that can either be applied directly for disease management, or be used as platforms to answer pertinent questions in medicine.
What do you enjoy doing in your spare time?
Outside the lab, I enjoy life chats with family and friends, engaging in mentorship and dancing, which has been an important part of my life since for as long as I can remember. I’ve been involved in Daffydil and the med Bollywood dance team as a dancer and choreographer over the last four years, and look forward to performing again in this year’s Daffy production! To be able to share my joy of dance with my family and friends in a way that also gives back to the community is special.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

University of Toronto Student Delivers First Virtual Reality Biochemistry Lecture
A University of Toronto graduate student is believed to be the first to use virtual reality in a biochemistry research lecture — allowing audience members to immerse themselves in 3D to better understand how the eye uses light to create vision.
Aidin Balo, a PhD student in the Department of Biochemistry, worked with the software company Autodesk and his PhD supervisor Professor Oliver Ernst to prepare the lecture. The team then supplied the audience with cheap cardboard-based tools they could use with their smartphones to instantly access an immersive atmosphere for peering deeply into the human eye.
“Anybody can do it,” says Balo. The software is public and you can make the glasses with cardboard and two pieces of convex glass. Then all you need is a desktop computer to prepare the content and a smartphone for each person. The goal here is to make virtual reality more accessible.”
Balo and Ernst delivered the lecture to 200 people in 2016 at a conference in Berlin, and then to a larger audience at ShanghaiTech University, with support from Autodesk’s Merry Wang and the Canadian Institute for Advanced Research. Based on good audience feedback, the three wrote about their experience in this month’s issue of the journal Nature Methods.
“So many people came up to us afterwards,” he says. “It was such an overwhelmingly positive experience that I was surprised.”
In his lecture, as Balo described how the visual pigment in the eye changes its shape and signals in response to light, his audience watched examples of these changes in real time. By looking up, down or sideways they could virtually circle around an entire protein, seeing the way it changed and how it worked in the eye. Balo realized that the experience made it easier for people outside his field of structural biology to understand how the first steps of vision work.
“Structural biologists would benefit from a virtual reality lecture, but so would those who are more interested in the bigger picture, but still need to know how molecules work,” he says. “Those could be biologists, chemists, physicists or even medical doctors.”
The Ernst lab at the Faculty of Medicine explores how light is converted to a chemical signal in the eye and how this signal is terminated. By understanding more about how the eye works to create vision, Balo hopes to learn more about when it fails to do so. He hopes that this research will contribute to future treatments for blindness.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Heidi Singer