U of T Researchers Demonstrate Safe and Non-invasive Way to open Blood-Brain Barrier in Patients with Alzheimer’s Disease
First peer-reviewed published report to show the safety and feasibility in Phase 1 trial
University of Toronto researchers have demonstrated that focused ultrasound can be used to safely open the blood-brain barrier (BBB) in patients with Alzheimer’s disease in the first peer-reviewed published report of its kind.

The study, “Blood-Brain Barrier Opening in Alzheimer’s Disease Using MR-guided Focused Ultrasound” has been published in Nature Communications.
“This is a critical first step,” says lead author Nir Lipsman, an assistant professor in the Department of Surgery and director of the Harquail Centre for Neuromodulation at Sunnybrook Health Sciences Centre. “By successfully, safely and reversibly opening the blood-brain barrier in patients with early-to- moderate Alzheimer’s disease, we can support the continued investigation of focused ultrasound as a potential novel treatment, and further study the delivery of therapies that otherwise cannot access the brain.”
The BBB surrounds the small blood vessels of the brain to protect it from toxins and infectious agents. It also prevents drug therapies from entering, which could be effective in treating disease. In this Phase 1 trial, the focused ultrasound technology used low frequency ultrasound waves to non-invasively open the BBB in a small area of the frontal lobe in patients with mild stage Alzheimer’s disease. No drug therapies were administered as the trial investigated safety and feasibility.
“While it is still early in development, in the future Focused Ultrasound may provide a non-invasive, effective way of delivering large molecules such as antibodies or even stem cells directly to the brain to help patients with Alzheimer’s,” says Professor Sandra Black, co-principal investigator and internationally renowned professor of Neurology at U of T and Sunnybrook. “We are pioneering exciting potential innovative treatment options for patients.”
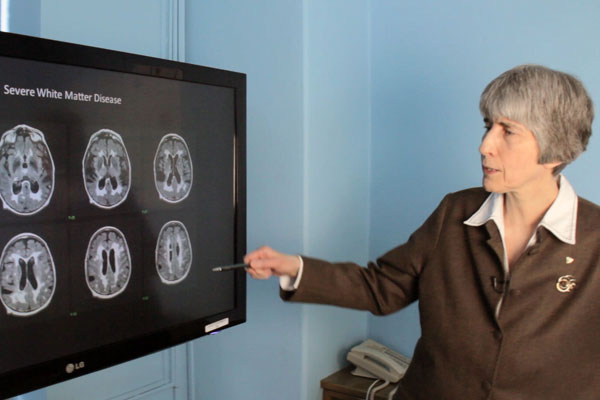
In 2015, Sunnybrook researchers safely opened the BBB to test the delivery of chemotherapy directly to a patient’s brain tumour. This recent study is the first peer-reviewed, published report showing the safety and feasibility of breaching the BBB in patients with Alzheimer’s.
Kullervo Hynynen, a professor of Medical Biophysics and Director of Physical Sciences at Sunnybrook Research Institute, worked with INSIGHTEC®, a global medical technology innovator of incisionless surgery, for almost two decades to develop the technology.
Alzheimer’s is the most common neurodegenerative disorder, which over time robs people of memory and thinking ability. Over 6.4 million people in North America and at least 44 million people worldwide, are living with Alzheimer’s or another dementia. Phase two of the study will begin this fall.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Remembering Dr. Hans Messner
Professor Hans Messner, a cherished physician who pioneered stem cell transplantation at Princess Margaret Cancer Centre and helped thousands of patients during his nearly 50-year career, died at the centre on July 24.
A professor of medical biophysics, Messner completed his PhD at the University of Toronto under the mentorship of Professor Ernest McCulloch. His early research focused on studying the "mother" cells that give rise to all other blood cells. Messner was part of McCulloch’s team that began to explore the potential benefits of bone marrow transplants for the treatment of patients with leukemia.
In 1976, Messner completed his first bone marrow transplant in which he transplanted stem cells collected from a matching donor to the patient to suppress the disease – in this case leukemia – and restore the patient's immune system. The procedure is formally known as an allogeneic transplant.
He went on to become a leader in the field of bone marrow transplantation. He developed and served as the first director of a clinical transplant program at the University Health Network’s Princess Margaret Cancer Centre (which was then called the Princess Margaret Hospital or PMH) and held the position of director of the Bone Marrow Transplant Centre until 2006. He was also a senior scientist at the Ontario Cancer Institute.
He was the founding president of the Canadian Bone Marrow Transplant Group and was a member of an expert working group that developed the Canadian Standard for Transplantation of Cells, Tissues and Organs. He also served as director of PMH’s Philip S. Orsino Cell Therapy Facility, where he developed the regulatory systems, supervised the facility construction and directed early clinical phases.
In 2007, Messner received the Canadian Blood Services Lifetime Achievement Award for being a pioneer of allogeneic bone marrow and stem cell transplantation in Canada.
Last year, he was presented with the American Society for Blood and Marrow Transplantation Lifetime Achievement Award, which recognizes people who have made continuous clinical and scientific contributions to the field.
In June, Messner reflected on his almost 50 years at the Princess Margaret as he inspired thousands of cyclists with a heartfelt message at the start of the annual Ride to Conquer Cancer, a fundraising event in which he was a rider for 10 years on his beloved "Heme Team."
Earlier this month, the stem cell transplantation program was renamed the Messner Allogeneic Transplant Program to honour his legacy.
Although Messner said he was retiring after 44 years, he never really did. In his final weeks, despite increasing frailty, he continued to come to work to consult with and advise his colleagues.
When one teased him saying, "I guess you're never going to retire." His reply, with a customary twinkle in his eye, was: "Might as well keep going!"
Funeral arrangements are still being finalized.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

The Intersection of Medicine, Media and Donald Trump
U of T researchers are warning the medical community that a popular cognitive test may be compromised due to the extensive publicity it received after U.S. President Donald Trump took it.

Recently, Trump’s physician announced that the President achieved a perfect score on the Montreal Cognitive Assessment (MoCA), a test for mild cognitive impairment, often the first step toward dementia. Media covered the story extensively, leading Faculty of Medicine researchers to investigate the impact this exposure could have on test-takers. One of the authors, Dr. Eric Coomes, a third-year medical resident in Internal Medicine, spoke with writer Heidi Singer about the study.
Why were you concerned about coverage of the MoCA?
Watching the news stories on the MoCA in relation to President Trump’s cognitive evaluation, we were impressed by the mass dissemination of information about this test that was primarily only known in the medical community until then. As readers were exposed to the test, and in some cases even being invited to self-administer the test online, we wondered if there could be an effect down the road. We wanted to quantify the degree and nature of the test’s dissemination.
We searched the news cycle for a period in January and found 190 articles in that time frame discussing the MoCA in association with President Trump. Of those, we found over half revealed either parts of or the full content of the MoCA questionnaire to the general public. More than one in six articles invited people to take the test, many posed as a self-challenge. A smaller proportion even provided answers so people could see how the test is graded.”
How problematic is that?
Previous studies have demonstrated a potential for a learning effect on the MoCA. It may be that your previous exposure will strengthen your future scores. The impact would likely be greatest among people with very mild cognitive impact. People with more severe cognitive impairment would be unlikely to remember having seen the answers to the test previously. But with people who are healthy or at the very earliest stages of cognitive impairment, there may be some effect. At this point, however, the risk associated with media dissemination is hypothetical. It would be interesting if future tests looked at this.
Is it best for health providers to avoid this test for the short term?
There’s an easy way out. All the articles presented version 1 of the test. There are other versions – 2 and 3 – that have different word lists and content. We published a letter in JAMA Neurology advising providers to ask people whether they’ve been previously exposed, and those who have, consider using alternate versions of the test.
For how long?
Depends whether there’s ongoing media interest on this test. This was the first time an American president underwent formal cognitive evaluation while in office, with mass media coverage. Only time will tell whether this will happen in the future. Until the learning effect of media coverage is better characterized, it hard to know how long an effect might last.
What kind of reaction have you received to your study?
We’ve all been impressed at how much interest there’s been of the study. There’s been a really positive response among our peers. There’s been quite a bit of local and international media interest. The goal of our piece was not to infer any conclusions about the President but rather to look at the impact of media dissemination of a cognitive evaluation.
Why do you think there has been so much interest?
It provided an impetus for lots of outlets to discuss the topic of the President’s cognitive testing. But it also gave some media an opportunity for self-reflection. The New York Times linked to their own previous coverage, in which they published contents of the questionnaire.
It was an excellent opportunity to explore the relationship between media and medicine and show how public-sphere events have an impact on clinical practice. The interplay between medicine and the general world is often overlooked, but as practitioners we need to be aware of that interplay. This is a perfect example of how they intersect.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

University of Toronto Scientists uncover DNA ‘shield’ with crucial roles in normal cell division, the immune system and cancer
Scientists have made a major discovery about how cells repair broken strands of DNA that could have exciting implications for the treatment of cancer.
Their study, published in Nature July 18, uncovered a brand new protein complex in cells that shields broken DNA ends and controls the way in which it is repaired.
The new complex pushes cancer cells to use a particular type of DNA repair system that is vulnerable to targeting by exciting new drugs called PARP inhibitors or platinum-based chemotherapies.
The landmark study was a result of collaboration between U of T, The Institute of Cancer Research, London, The Netherlands Cancer Institute and the University of Bern.
The discovery could lead to tests to direct and monitor treatment for patients with mutations in BRCA1, BRCA2 or other DNA repair genes, treated with platinum-based chemotherapies or exciting new drugs called PARP inhibitors.
“PARP inhibitors hold great promise for breast and ovarian cancer treatment, but we must understand why they sometimes don't work, or stop working altogether,” says Daniel Durocher, a professor in the Department of Molecular Genetics and Senior Investigator in the Lunenfeld-Tanenbaum Research Institute at the Sinai Health System. “Knowing more about how cancer evades PARP inhibition by studying basic DNA repair mechanisms brings us a big step closer to this objective, which will improve how we treat some of the most intractable cancers."
The newly named ‘Shieldin’ complex was also found to be important for generating the right type of antibodies during an immune response, and mutations could lead to immune-related disorders.
PARP inhibitors are hugely promising treatments because they take advantage of a major vulnerability of some cancers – a weakness in the ability of cancer cells to repair their DNA. Traditional platinum-based chemotherapies are also being used in a more targeted way to take advantage of DNA repair weaknesses.
When intact, the newly discovered Shieldin complex was found to contribute to this vulnerability by attaching to the broken DNA, forcing cancer cells to attempt to repair their DNA in a way that makes them susceptible to PARP inhibitors and platinum chemotherapies.
But when mutations are introduced in the components of the complex, the researchers found that cancer cells grown in the lab and in mice used an alternative way to repair DNA and quickly became resistant to PARP inhibitors.
The PARP inhibitor drug olaparib is approved in the US and Europe for treating ovarian and breast cancers with BRCA mutations, and looks promising against some prostate cancers – so the results could have a wide impact on cancer treatment if mutations in the ‘Shieldin’ complex are shown to lead to treatment failure in the clinic.
To uncover the complex, the international team of researchers analysed breast cancer cells and mice that had mutations in the gene BRCA1.
They used cutting-edge Crispr/Cas9 genetic manipulation technology to search for gene mutations that caused cells to become resistant to the PARP inhibitor drugs olaparib and talaoparib, as well as the platinum chemotherapy cisplatin.
Through painstaking experiments, the researchers were able to pick out key gene mutations that led to drug resistance, which proteins these had an effect on, and work out what these proteins did in cells.
They found the new complex is composed of newly identified proteins, now named SHLD1, SHLD2, and SHLD3.
In healthy cells, the complex was found to attach to the ends of broken DNA so that the ‘blunt ends’ of the DNA have to be stuck back together directly – a quicker, messier way of repairing DNA that can sometimes be necessary for making antibodies during immune responses.
When the researchers introduced mutations into the Shieldin complex – which stop it from forming and protecting broken DNA ends – cells are free to repair DNA via a different method, and this means PARP inhibitors are no longer effective.
The study was funded by a variety of organizations worldwide, including Canadian Cancer Society and the Canadian Institutes of Health Research, and Cancer Research UK and Breast Cancer Now in the UK.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Evaluating Residents By Competency, Not Time
As medical residencies begin this week, the learning and evaluation process is significantly different in six specialties, including Medical Oncology and Emergency Medicine.
That’s because medical education in Canada is moving to an increasingly customized, intimate teaching approach, with more frequent testing, more hands-on support and supervision by senior physicians, and a greater focus on communication skills such as the ability to deliver bad news to patients. Dubbed “Competence by Design (CBD),” the new format was pioneered at U of T, and is being gradually implemented in every medical school in Canada.
In specialties that have made the switch, such as Otolaryngology, learning is less about logging a certain number of hours, and more about showing – in real time -- that necessary ‘competencies’ have been acquired.
“Now we’re highlighting the skills and professional activities that make up our skillset and signing off on each one as our learners acquire them,” says Professor Paolo Campisi, Vice Chair Education and Director of Postgraduate Education for the Department of Otolaryngology – Head & Neck Surgery. “We test constantly, so each test is lower-stakes, and we intervene early to correct any deficiencies.”
Although it’s very rare for a resident to fail their final exams in the current system, Campisi says correcting problems as soon as they come up is better, since residents are delivering care throughout their learning process. So, if a resident struggles to deliver bad news with clear, compassionate communication skills, that problem will be addressed immediately, benefitting his or her next patient. “The ultimate goal is to make things better for patients,” Campisi says.
Medical students are highly accomplished, and educators have realized, with concern, that many never experienced failure until they reached the high-stakes environment of medicine. Yet, learning to fail – among other ‘soft skills’ is considered important to avoid burnout and other problems.
Marissa Bonyun, a fourth-year resident in Orthopaedic Surgery, likes being evaluated in real time in the workplace because “it gives us the opportunity to become accustomed not just to performing and testing, but also to gauge where we are on a regular basis,” she says. “As adult learners, this more frequent testing puts the focus on constant improvement and making learning goals to achieve and work towards. It’s more of a focus on testing forlearning rather than oflearning.”
 U of T’s Faculty of Medicine pioneered the new style of learning in its Department of Orthopaedic Surgery almost a decade ago. The Department of Family Medicine was also an early adopter. Last year, the Royal College of Physicians and Surgeons, working with Canada’s 17 medical schools, officially rolled out the CBD program for Otolaryngology and Anesthesiology across Canada. This year, the six specialties to sign on are: Emergency Medicine, Forensic Pathology, Medical Oncology, Nephrology, Surgical Foundations, and Urology. A dozen more will make the switch next year. Eventually, 65 specialties will educate residents using the CBD model.
U of T’s Faculty of Medicine pioneered the new style of learning in its Department of Orthopaedic Surgery almost a decade ago. The Department of Family Medicine was also an early adopter. Last year, the Royal College of Physicians and Surgeons, working with Canada’s 17 medical schools, officially rolled out the CBD program for Otolaryngology and Anesthesiology across Canada. This year, the six specialties to sign on are: Emergency Medicine, Forensic Pathology, Medical Oncology, Nephrology, Surgical Foundations, and Urology. A dozen more will make the switch next year. Eventually, 65 specialties will educate residents using the CBD model.
“It has been gratifying to see more and more interest among our faculty members and learners and requests to be involved in CBD,” says Professor Glen Bandiera, Associate Dean, Postgraduate Medical Education, who is overseeing its implementation at the Faculty of Medicine. “It’s important we make sure to support everyone in this process, so we’re working with U of T’s Centre for Faculty Development to offer training to faculty in particular on coaching and providing effective feedback. And just as the new model trains learners to respond to feedback and be flexible with change, we at the Faculty leadership level will be listening to everyone involved and making adjustments as necessary.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Heidi Singer

Canada Honours Faculty of Medicine Researchers
 Six members of the Faculty of Medicine have been named to the Order of Canada.
Six members of the Faculty of Medicine have been named to the Order of Canada.
They are among the 105 new appointments announced by Her Excellency the Right Honourable Julie Payette, Governor General of Canada on June 29.
University Professor Peter Henry St George-Hyslop, of the Department of Medicine, was named Officer of the Order of Canada. The appointment recognizes St George-Hyslop’s research on the role of genetics in neural degeneration. His work has advanced our understanding of neurodegenerative disorders, notably Alzheimer’s disease.
One of the world’s leading neurodegenerative disease investigators, St George-Hyslop is Director of the Tanz Centre for Research in Neurodegenerative Diseases. He has discovered key genes and proteins that cause cells to degenerate in diseases like early-onset Alzheimer’s disease, and also demonstrated that a variety of genetic and non-genetic factors contribute to Alzheimer’s. His work has been cited by other researchers more than 33,000 times.
Last year, St George-Hyslop was awarded the Ryman Prize, the world’s richest prize established as an honour equivalent to a Nobel Prize for people working in the field of health of older adults.
The five other appointees from across the Faculty were named Members of the Order of Canada (C.M.)
Allan Steven Detsky
Department of Medicine, Division of General Internal Medicine
For his advanced economic expertise in the Canadian healthcare system, notably with respect to clinical policy making through cost-effective enhancements to improve patient outcomes.
Mitchell Halperin
Department of Medicine, Division of Nephrology
For his renowned leadership within the field of nephrology as a clinician, researcher and educator.
K. Wayne Johnston
Department of Surgery, Division of Vascular Surgery
For his foundational leadership within the field of vascular surgery in Canada as a surgeon, researcher and educator.
Bryce Taylor
Department of Surgery, Division of General Surgery
For his sustained impact on the teaching and practice of surgery in Canada, notably as an advocate for improving surgical safety standards and patient care.
James Patterson Waddell
Department of Surgery, Division of Orthopaedic Surgery
For his sustained leadership within the field of orthopaedic surgery and for his dedication in advancing best practices in orthopaedic care across Canada.
The Order of Canada recognizes outstanding achievement, dedication to the community and service to the country. A ceremony will be held at a later date for recipients to accept their insignia.
To read more about more of this year’s Order of Canada inductees at the University of Toronto, click here. To view a full list of the appointments, click here.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.

The Eyes: Windows to Our Health
It’s said that the eyes are windows to the soul. But to Professors Yeni Yucel and Neeru Gupta and their research team, the eyes are windows to our health.

In 2009, Yucel and his team found that contrary to popular belief, the human eye has a lymphatic system. This system is responsible for clearing fluid and waste out of tissues. The inability to clear fluid from the eye causes a buildup of pressure, and pressure is the main cause of glaucoma.
“Since then, our contribution has been to look at the implications of this completely new system for eye health, vision, and disease,” said Yucel, a professor of Opthalmology and Laboratory Medicine and Pathobiology, and a pathologist at St. Michael’s Hospital.
Most recently, in a paper published in early June, the team of researchers found that in vivo photoacoustic imaging – a technique that allows for very high-resolution imaging of a live model – can be used to measure fluid movement from inside the eye to the neck’s lymph nodes. This novel work proved that fluid from the eye drains at least in part to the larger lymphatic system, tying the eye to the larger fluid flow in the body.
Another study in late 2017 revealed a previously unknown pathway through which cerebrospinal fluid – the water around the brain – enters the optic nerve. This has added to the body of knowledge around the glymphatic system – the waste clearance pathway of the central nervous system – and has contributed a new perspective to glaucoma research.
Glaucoma is one of the world’s leading causes of irreversible blindness. Often undetected in its onset, once a patient receives the diagnosis, progressive vision loss is inevitable, although it can be slowed with treatments to lower pressure in the eye.
“We really don’t know what causes glaucoma,” says Gupta, also a professor of Opthalmology and Laboratory Medicine and Pathobiology, a clinician-scientist at St. Michael's and co-primary investigator of these studies. “We know there’s a problem with the drainage system of the eye and fluids not getting out. These discoveries open up a brand new window – now we can look at whether the problem in glaucoma is a lack of waste clearing, or an issue with this glymphatic system.”

The team's discoveries will also help test the efficacy of new medications for diseases such as glaucoma, and look at other targets to treat the eye.
“Everything we do has the patient at the centre,” says Gupta, director of the Glaucoma Unit at St. Michael’s, and a member of the Board of Directors of the World Glaucoma Association.
“There would be no excitement in any of this research if we didn’t feel it was deeply connected to the patients who sit in our exam rooms every day.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Autobahns for DNA ambulances
 Understanding precisely how damaged DNA gets repaired is an important avenue in developing better treatments for various diseases such as cancer.
Understanding precisely how damaged DNA gets repaired is an important avenue in developing better treatments for various diseases such as cancer.
Molecular biologists at work in this field sought fresh insight recently from a non-traditional source: University of Toronto’s Institute for Aerospace Studies. The results – published in Nature Communications this week – shed light on the movement of damaged DNA within the nucleus of the cell, a key step in the repair process.
The unusual biology-aerospace collaboration arose when U of T Medicine Prof. Karim Mekhail, Canada Research Chair in Spatial Genome Organization, ran up against a tricky problem trying to detect the directional motion of damaged DNA. (Like many scientists he often uses yeast cells for their similarity to the human genome, their ease of use and low cost.)
Keep in mind the genome is not a static set of biochemical instructions. It exists in a dynamic environment inside the nuclei of our cells – and the action of repair machinery goes into high gear when a piece of DNA is damaged by chemicals or radiation, for example. Understanding these mechanisms can help refine targets for improved cancer therapies.
“If you know that a key step of DNA repair is critical to our ability to treat cancer but you think this step is random, it is hard to design rational, targeted therapeutics or to improve upon our current therapies,” said Mekhail, an associate professor in the Department of Laboratory Medicine and Pathobiology.
Mekhail’s team had previously shown how damaged DNA is transported to specialized parts of the nucleus that act as DNA “hospitals”, areas enriched in DNA repair factors. Transporting the DNA to those areas are motor proteins that act as DNA “ambulances”.
In the new study from Mekhail’s team, first-author and PhD student Roxanne Oshidari used super-resolution microscopy and found that the “ambulances” transport damaged DNA along “highways” that are built on-demand from filamentous proteins called microtubules.
“This was very exciting as it suggested that damaged DNA can exhibit directional motion – not just random mobility as previously thought,” said Oshidari. But the microtubule highways are themselves also moving, making the calculations tricky to separate the motion of the damaged DNA transported by “ambulances” from the oscillating motion of the “highways”. This sent Mekhail on the hunt for the right collaborator.
“We looked across the globe for experts in single particle motion physics and were happy to find that world-renowned experts in that field are actually aerospace engineers here at the University of Toronto Institute for Aerospace Studies,” said Mekhail. He sent an email to Institute Director Christopher Damaren and was delighted with the response.
“Immediately, Chris was highly enthusiastic and demonstrated a true passion for the problem. We had several meetings in which we went over all of the data and brainstormed possible solutions. Side conversations often centered on the similarities and differences between our experience as biomedical researchers and their experience as aerospace engineers specializing in spacecraft motion physics.”
After a number of meetings – and a lot of thinking – Mekhail said it became apparent that the underlying problem is that biomedical researchers are over-reliant on mathematical equations that can detect directional motion only if it is perfectly linear: “This is because the traditional equations try to deduce the direction of motion from the assessment of distances travelled. In contrast, Chris helped us calculate whether damaged DNA moves following angles that result in directional motion, whichis close to but may not be perfectly linear.”
This approach allowed Mekhail and his team to readily detect – for the first time – the directional motion of damaged DNA both at the single cell level as well as the cell population level. It also helped them demonstrate that damaged DNA exhibits a very wide range of speeds as it is being transported; those microtubule highways are more like speed-limitless “autobahns” than controlled speed highways.
They have also examined which cellular factors help promote or repress this movement – and are looking at tools to modulate these factors to make cancer therapies more effective.
Mekhail is confident this unique aerospace engineering-biology collaboration will continue to decipher biomedical secrets. The positive outlook is shared by Damaren: “As we continue to work at the intersection of our fields, we are exploring how the application of our approaches to the study of biological problems may help tweak and refine these approaches, to the benefit of both biological and aerospace applications.”
This research was funded by the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, and the Ontario Early Researcher Award.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Linda Quattrin

Psychiatric Disorders Share an Underlying Genetic Basis
U of T Researchers Contribute to Landmark International Paper
Nine researchers from U of T’s Faculty of Medicine contributed to a major international study, published in the journal Science, showing the underlying genetic similarities between mental illnesses like schizophrenia and bipolar disorder.

The team, led by Harvard University’s Broad Institute, determined that psychiatric disorders share many genetic variants, while neurological disorders such as Parkinson’s or Alzheimer’s appear more distinct.
The study takes the broadest look yet at how genetic variation relates to brain disorders -- and highlights the power of large international collaborations to amplify Canada's investment in research.
The results indicate that psychiatric disorders likely have important similarities at a molecular level, even though they have always been considered separate diseases.
“Because these diseases look and act differently, we’ve always assumed they were different genetically too – that there would be a gene, or group of genes, for schizophrenia, and a gene or a group of genes for autism, and so on,” says Russell Schachar, a professor in U of T’s Department of Psychiatry and a co-author of the paper. “A cake and a flan have similar ingredients, but the result is different because of the way they’re put together. We didn’t expect psychiatric disorders that are so different to have such similar ‘ingredients.’
Only about five years ago, scientists started to see significant genetic overlap between psychiatric diseases, says Schachar. Understanding what a broad spectrum of mental health conditions share might hasten better treatments in particular for the most intractable and serious diseases, like schizophrenia.
U of T contributors to the paper include Alzheimer’s researchers Professors Peter St. George-Hyslop and Ekaterina Rogaeva; Tourette syndrome researchers Professors Cathy Barr and Paul Sandor; ADHD researcher Assistant Professor Jennifer Crosbie, OCD researcher Associate Professor Margaret Richter, autism researcher Professor Stephen Scherer, along with Professors Jacob Vorstman and Schachar, who study the confluence of ADHD and autism.

The unprecedented scope of international cooperation could be a model for Canadian researchers, says Scherer, because the vast landscape of interconnected scientists in this country, could one day produce the next landmark genetic research of grand scale. Scherer is Director of U of T's McLaughlin Centre and a Senior Scientist at The Hospital for Sick Children (SickKids).
“It showed the capacity of scientists around the world to work together,” he says. “We hope Canadian funding agencies might decide to fund population-scale cohort studies, instead of us shipping our samples and data to the USA. Toronto can and should be a central hub for this kind of work going forward.”
For the current study, international consortia pooled their data to examine the genetic patterns across 25 psychiatric and neurological diseases. Because each genetic variant only contributes a tiny percentage of the risk for developing a given disorder, the analyses required huge sample sizes to separate reliable signals from noise.
The researchers measured the amount of genetic overlap across the disorders of 265,218 patients and 784,643 controls. They also examined the relationships between brain disorders and 17 physical or cognitive measures, such as years of education, from 1,191,588 individuals.
The final results indicated widespread genetic overlap across different types of psychiatric disorders, particularly between attention-deficit/hyperactivity disorder (ADHD), bipolar disorder, major depressive disorder, and schizophrenia. The data also indicated strong overlap between anorexia nervosa and obsessive-compulsive disorder (OCD), as well as between OCD and Tourette syndrome.
In contrast, neurological disorders such as Parkinson’s and multiple sclerosis appeared more distinct from one another and from the psychiatric disorders — except for migraine, which was genetically correlated to ADHD, major depressive disorder, and Tourette syndrome.
According to the researchers, the high degree of genetic correlation among the psychiatric disorders suggests that current clinical categories do not accurately reflect the underlying biology. “The tradition of drawing these sharp lines when patients are diagnosed probably doesn’t follow the reality, where mechanisms in the brain might cause overlapping symptoms,” says Neale.
As a hypothetical example, a single mechanism regulating concentration could drive both inattentive behavior in ADHD and diminished executive function in schizophrenia. Further exploration of these genetic connections could help define new clinical phenotypes and inform treatment development and selection for patients.
Additionally, within the cognitive measures, the researchers were surprised to note that genetic factors predisposing individuals to certain psychiatric disorders — namely anorexia, autism, bipolar disorder, and OCD — were significantly correlated with factors associated with higher childhood cognitive measures, including more years of education and college attainment. Neurological disorders, however, particularly Alzheimer’s and stroke, were negatively correlated with those same cognitive measures.
“We were surprised that genetic factors of some neurological diseases, normally associated with the elderly, were negatively linked to genetic factors affecting early cognitive measures,” says Verneri Anttila, a postdoctoral research fellow at Harvard’s Broad Institute, the paper’s first author. “It was also surprising that the genetic factors related to many psychiatric disorders were positively correlated with educational attainment. We’ll need more work and even larger sample sizes to understand these connections.”
The consortia have made their data accessible online.
With files from Karen Zusi, Broad Institute of MIT and Harvard.

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Heidi Singer

The ‘Write’ Elective for Residents
Medical residents with an interest in communications can now take an elective honing their writing skills for U of T-linked website Healthy Debate.
“It’s a cool hybrid between academic writing and writing for a general audience,” says Wilson Kwong, a third-year resident in internal medicine who, in August, will become the first Faculty of Medicine learner to take the elective. “Storytelling and writing is something I’m interested in, and it seems to align with my career goals because wherever I end up practicing, I’m hoping to do more writing.”

Professor Andreas Laupacis, a general internist, created the website six years ago, primarily as a high-quality journalism resource for health professionals. It was originally headquartered at St. Michael’s Hospital, where he was executive director of the Li Ka Shing Knowledge Institute. Since stepping down from that role, Laupacis has moved Healthy Debate to U of T’s Department of Medicine, where he has become Lead, Patient Involvement. At U of T, he is eager to spend more time building it into a resource for both medical workers and patients.
“The editorial board composition is now about 50 percent patients,” says Laupacis. “I made a very deliberate decision to ask people with diverse experiences with the health system: a young man who is quadraplegic, dependent on a ventilator and lives at home; a mom whose child spent the first year-and-a-half in the NICU; a person who has bipolar disorder, and a woman who is indigenous (Saulteaux from the Peguis nation) , among others. I expect the patients will push us to do different kinds of stories than we’ve done to date.”
During the month of their placement with Healthy Debate, each resident will be expected to complete a minimum of one article, one opinion piece and one profile of a health provider, as part of the popular Faces of Health Care series.
Kwong is particularly interested in using journalism skills to explore long-term care for elderly people in Toronto across different cultures.
“I have grandparents who had great experiences in Chinese nursing homes in the GTA,” he says. “I’d like to see if other cultures around the city have these types of nursing homes and whether people value them.”
The website receives around 100,000 visits per month. University students make up a significant part of the readership, and Laupacis hopes the addition of residents will further this readership. Dr. Seema Marwaha, a general internist at Trillium Health Partners, is a member of the Healthy Debate editorial board and has experience with multimedia approaches (e.g. podcasting, video). She will help interested residents develop multimedia, adding to the website’s storytelling scope.
“I have a feeling residents will bring a different vibe to the whole thing,” Laupacis says.

Kwong has written for publications such as CMAJ previously, and believes the skills that come with journalism – interviewing, listening, and developing narratives – will further his medical education.
“The more articles you write, the more you get to talk to patients, absorb their stories and share in some way,” he says, “ I think makes you a better doctor.”

Optimize this page for search engines by customizing the Meta Title and Meta Description fields.
Use the Google Search Result Preview Tool to test different content ideas.

Select a Meta Image to tell a social media platform what image to use when sharing.
If blank, different social platforms like LinkedIn will randomly select an image on the page to appear on shared posts.
Posts with images generally perform better on social media so it is worth selecting an engaging image.
Heidi Singer
